Online first
Bieżący numer
Archiwum
O czasopiśmie
Polityka etyki publikacyjnej
System antyplagiatowy
Instrukcje dla Autorów
Instrukcje dla Recenzentów
Rada Redakcyjna
Komitet Redakcyjny
Recenzenci
Wszyscy recenzenci
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
Kontakt
Bazy indeksacyjne
Klauzula przetwarzania danych osobowych (RODO)
PRACA ORYGINALNA
Korelaty podatności na używanie tytoniu wśród nigdy niepalącej młodzieży w czterech krajach Europy Wschodniej i Południowej
1
Medical University, Łódź, Poland
Autor do korespondencji
Med Og Nauk Zdr. 2023;29(3):196-204
SŁOWA KLUCZOWE
DZIEDZINY
STRESZCZENIE
Wprowadzenie i cel:
Palenie papierosów i e-papierosów jest najbardziej rozpowszechnione wśród młodych dorosłych, co uzasadnia prowadzenie w tej grupie badań w celu identyfikacji korelacji dotyczących stosowania tych używek. Celem przeprowadzonego przez autorów niniejszej pracy badania było porównanie korelatów związanych z podatnością na palenie wśród młodzieży w czterech krajach Europy Wschodniej i Południowej.
Materiał i metody:
Analizie poddano najnowsze dane z GYTS, uzyskane na Łotwie (2019), w Mołdawii (2019), Czarnogórze (2018) i San Marino (2018). Narzędziem badawczym był wystandaryzowany, anonimowy kwestionariusz ankiety, składający się z pytań dotyczących cech społeczno-demograficznych, rozpowszechnienia palenia tytoniu, wiedzy i postaw młodzieży wobec palenia, dostępu do papierosów, roli reklamy i mediów w paleniu tytoniu.
Wyniki:
Prawie 1/3 młodych dorosłych była skłonna do palenia w San Marino, a 1/4 na Łotwie. We wszystkich czterech analizowanych krajach narażenie na bierne palenie (SHS) w miejscach publicznych było predyktorem podatności na palenie tytoniu (OR od 1,4 do 1,79; p < 0,01 w Czarnogórze; p < 0,001 w Mołdawii). W trzech analizowanych krajach korelatami były: ekspozycja na SHS w domu (OR 1,31; p < 0,05 na Łotwie; OR 1,51; p < 0,01 w Mołdawii; OR 1,91; p < 0,01 w San Marino), poczucie komfortu (OR 1,59; p < 0,001 na Łotwie; OR 1,45; p < 0,01 w Mołdawii; OR 1,41; p < 0,01 w Czarnogórze) oraz opinia, że palacz może łatwo rzucić palenie (OR 1,39; p < 0,05 na Łotwie; OR 1,84; p < 0,001 w Mołdawii; OR 1,4; p < 0,05 w Czarnogórze).
Wnioski:
Czynniki polityczne (przestrzeganie zakazów palenia w miejscach publicznych i domach) były silnie skorelowane z podatnością na używanie tytoniu. Wyniki te powinny zwrócić uwagę rządów i zintensyfikować interwencje zachęcające do wprowadzania domów wolnych od tytoniu oraz kontrole zakazów palenia w miejscach publicznych.
Palenie papierosów i e-papierosów jest najbardziej rozpowszechnione wśród młodych dorosłych, co uzasadnia prowadzenie w tej grupie badań w celu identyfikacji korelacji dotyczących stosowania tych używek. Celem przeprowadzonego przez autorów niniejszej pracy badania było porównanie korelatów związanych z podatnością na palenie wśród młodzieży w czterech krajach Europy Wschodniej i Południowej.
Materiał i metody:
Analizie poddano najnowsze dane z GYTS, uzyskane na Łotwie (2019), w Mołdawii (2019), Czarnogórze (2018) i San Marino (2018). Narzędziem badawczym był wystandaryzowany, anonimowy kwestionariusz ankiety, składający się z pytań dotyczących cech społeczno-demograficznych, rozpowszechnienia palenia tytoniu, wiedzy i postaw młodzieży wobec palenia, dostępu do papierosów, roli reklamy i mediów w paleniu tytoniu.
Wyniki:
Prawie 1/3 młodych dorosłych była skłonna do palenia w San Marino, a 1/4 na Łotwie. We wszystkich czterech analizowanych krajach narażenie na bierne palenie (SHS) w miejscach publicznych było predyktorem podatności na palenie tytoniu (OR od 1,4 do 1,79; p < 0,01 w Czarnogórze; p < 0,001 w Mołdawii). W trzech analizowanych krajach korelatami były: ekspozycja na SHS w domu (OR 1,31; p < 0,05 na Łotwie; OR 1,51; p < 0,01 w Mołdawii; OR 1,91; p < 0,01 w San Marino), poczucie komfortu (OR 1,59; p < 0,001 na Łotwie; OR 1,45; p < 0,01 w Mołdawii; OR 1,41; p < 0,01 w Czarnogórze) oraz opinia, że palacz może łatwo rzucić palenie (OR 1,39; p < 0,05 na Łotwie; OR 1,84; p < 0,001 w Mołdawii; OR 1,4; p < 0,05 w Czarnogórze).
Wnioski:
Czynniki polityczne (przestrzeganie zakazów palenia w miejscach publicznych i domach) były silnie skorelowane z podatnością na używanie tytoniu. Wyniki te powinny zwrócić uwagę rządów i zintensyfikować interwencje zachęcające do wprowadzania domów wolnych od tytoniu oraz kontrole zakazów palenia w miejscach publicznych.
Introduction and objective:
Young adults demonstrate the highest prevalence of cigarette and e-cigarette use which justifies conducting research in attempt to identify correlates of the use of cigarettes and e-cigarettes. The aim of the study was to compare predictors related to smoking susceptibility among adolescents in four Eastern and Southern European countries.
Material and methods:
The latest data from the Global Youth Tobacco Survey (GYTS), obtained from Latvia (2019), Moldova (2019), Montenegro (2018), and San Marino (2018) were subject to analysis. The research tool was a standardized, anonymous survey questionnaire, consisting of basic questions regarding socio-demographic characteristics, prevalence of tobacco smoking, knowledge and attitudes of young people about and to smoking, access to cigarettes, the role of advertising and the media in tobacco smoking.
Results:
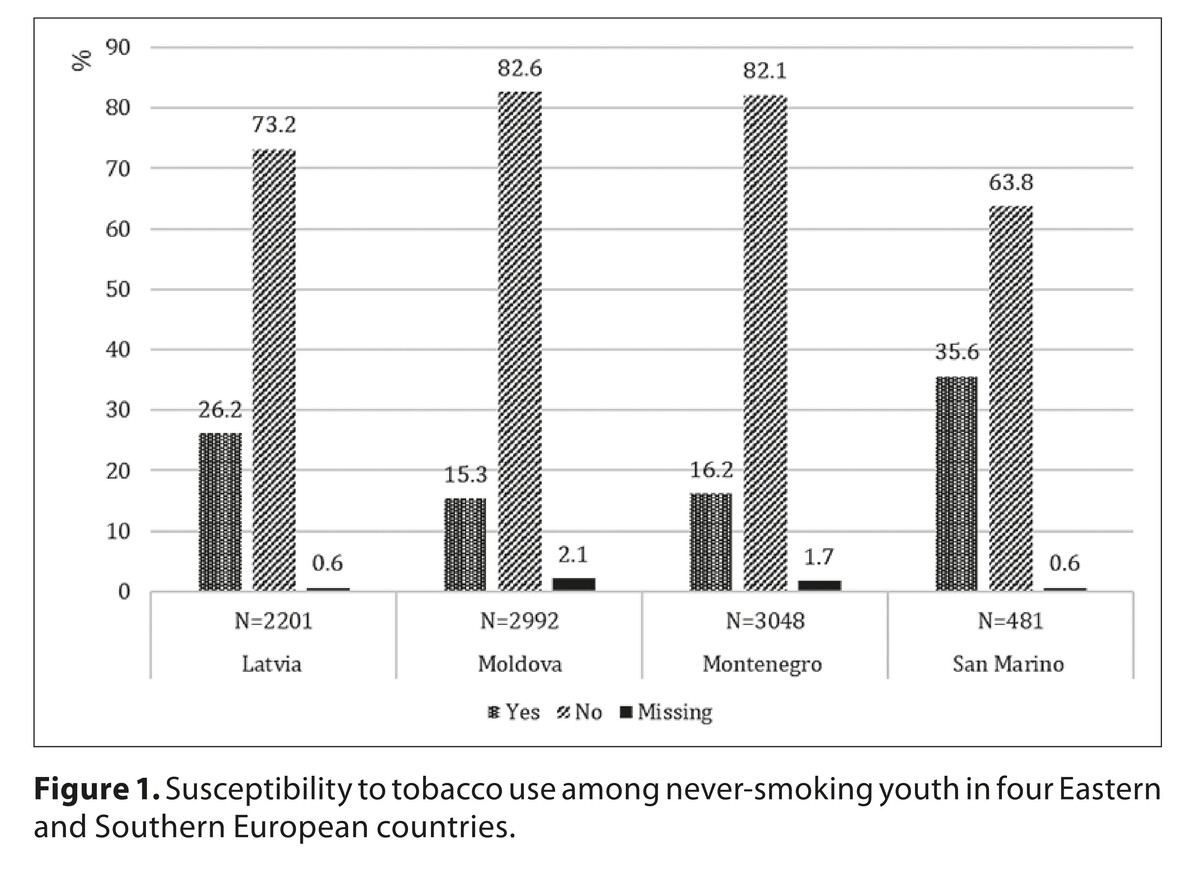
Nearly one-third of young adults were prone to smoking in San Marino and a one-fourth in Latvia. In all four analyzed countries, exposure to second-hand smoke (SHS) in public places was a predictor of vulnerability to tobacco use (OR 1.4 – 1.79; p<0.01 in Montenegro; p<0.001 in Moldova). In three analyzed countries, the correlates were: exposure to SHS at home (OR 1.31; p<0.05 in Latvia; 1.51; p<0.01 in Moldova; 1.91; p<0.01 in San Marino), the feeling of comfort (OR 1.59; p< 0.001 in Latvia; 1.45; p< 0.01 in Moldova; 1.41; p< 0.01 in Montenegro), and the opinion that a smoker can easily quit smoking (OR 1.39; p< 0.05 in Latvia; 1.84; p< 0.001 in Moldova; 1.4; p<0.05 in Montenegro).
Conclusions:
Political factors (observance of smoking bans in public places and homes) were strongly correlated with tobacco use susceptibility. These results should induce governments to intensify interventions to encourage tobacco-free homes, and control smoking bans in public places.
Young adults demonstrate the highest prevalence of cigarette and e-cigarette use which justifies conducting research in attempt to identify correlates of the use of cigarettes and e-cigarettes. The aim of the study was to compare predictors related to smoking susceptibility among adolescents in four Eastern and Southern European countries.
Material and methods:
The latest data from the Global Youth Tobacco Survey (GYTS), obtained from Latvia (2019), Moldova (2019), Montenegro (2018), and San Marino (2018) were subject to analysis. The research tool was a standardized, anonymous survey questionnaire, consisting of basic questions regarding socio-demographic characteristics, prevalence of tobacco smoking, knowledge and attitudes of young people about and to smoking, access to cigarettes, the role of advertising and the media in tobacco smoking.
Results:
Nearly one-third of young adults were prone to smoking in San Marino and a one-fourth in Latvia. In all four analyzed countries, exposure to second-hand smoke (SHS) in public places was a predictor of vulnerability to tobacco use (OR 1.4 – 1.79; p<0.01 in Montenegro; p<0.001 in Moldova). In three analyzed countries, the correlates were: exposure to SHS at home (OR 1.31; p<0.05 in Latvia; 1.51; p<0.01 in Moldova; 1.91; p<0.01 in San Marino), the feeling of comfort (OR 1.59; p< 0.001 in Latvia; 1.45; p< 0.01 in Moldova; 1.41; p< 0.01 in Montenegro), and the opinion that a smoker can easily quit smoking (OR 1.39; p< 0.05 in Latvia; 1.84; p< 0.001 in Moldova; 1.4; p<0.05 in Montenegro).
Conclusions:
Political factors (observance of smoking bans in public places and homes) were strongly correlated with tobacco use susceptibility. These results should induce governments to intensify interventions to encourage tobacco-free homes, and control smoking bans in public places.
Wężyk-Caba I, Znyk M. Correlates of susceptibility to tobacco use among never-smoking youth in four eastern and southern European
countries. Med Og Nauk Zdr. 2023; 29(3): 196–204. doi: 10.26444/monz/169770
REFERENCJE (72)
1.
GBD 2015 Tobacco Collaborators. Smoking prevalence and attributable disease burden in 195 countries and territories, 1990–2015: A systematic analysis from the Global Burden of Disease Study 2015. Lancet. 2017;389(10082):1885–1906. doi:10.1016/S0140-6736(17)30819-X.
3.
Ljaljević A, Zvrko E, Stojiljković M. Tobacco Use Among Youth: Findings from the Global Youth Tobacco Survey in Montenegro. Arh Hig Rada Toksikol. 2008;59(3)183–189. https://doi.org/10.2478/10004-....
4.
Smoking in Europe: Which countries are the most and least addicted to tobacco and vaping? https://www.euronews.com/next/.... (access: 2023.05.01).
5.
WHO global report on trends in prevalence of tobacco use 2000–2025. 4th edition. Geneva: World Health Organization; 2021.
6.
Gallus S, Lugo A, Liu X, Behrakis P, et al. Who smokes in Europe? Data from 12 European countries in the TackSHS survey (2017–2018). J Epidemiol. 2021;31(2):145–151. doi:10.2188/jea.JE20190344.
7.
Hamzeh B, Farnia V, Moradinazar M, et al. Pattern of cigarette smoking: Intensity, cessation, and age of beginning. Evidence from a cohort study in West of Iran. Subst Abus Treat Prev Policy. 2020;15:83. https://doi.org/10.1186/s13011....
8.
Kashyap S. Smoking Among Teenagers with Emphasis on Social Marketing as a Solution. Int J Res Publ Rev. 2021;8(2):964–968.
9.
Kim N, Loh WY, McCarthy DE. Machine learning models of tobacco susceptibility and current use among adolescents from 97 countries in the Global Youth Tobacco Survey, 2013–2017. PLOS Glob Public Health. 2021;1(12):e0000060. doi:10.1371/journal.pgph.0000060.
10.
Marcon A, Pesce G, Calciano L, et al. Trends in smoking initiation in Europe over 40 years: A retrospective cohort study. PLoS ONE 2018;13(8):e0201881. doi:10.1371/journal.pone.0201881.
11.
WHO Report on the global tobacco epidemic, 2019. Offer help to quit tobacco use. Geneva: World Health Organization; 2019.
12.
O’Brien D, Long J, Quigley J, et al. Association between electronic cigarette use and tobacco cigarette smoking initiation in adolescents: a systematic review and meta-analysis. BMC Public Health. 2021;21:954. doi: 10.1186/s12889-021-10935.
13.
Jones DM, Guy MC, Fairman BJ, et al. Nicotine Dependence among Current Cigarette Smokers Who Use E-Cigarettes and Cannabis. Subst Use Misuse, 2023;58(5):618–628. doi:10.1080/10826084.2023.2177961.
14.
Evans DS, O’Farrell A, Sheridan A, et al. Social Connectedness and Smoking among Adolescents in Ireland: An Analysis of the Health Behaviour in Schoolchildren Study. Int J Environ Res Public Health. 2023;20(9):5667. https://doi.org/10.3390/ijerph....
15.
Lim Y-S, Lee JY. A Comparative Analysis of E-Cigarette and Cigarette Posts on Instagram. Int J Environ Res Public Health. 2023;20(4):3116. https://doi.org/10.3390/ijerph....
16.
Meschack AF, Hu S, Pallone UE, et al. Texas tobacco prevention pilot initiative: process and effects. Health Educ Res. 2004;19(6):657–68. doi:10.1093/her/cyg088.
17.
Frech A. Healthy behavior trajectories between adolescence and young adulthood. Adv Life Course Res. 2012;17(2):59–68. doi: 10.1016/j.alcr.2012.01.003.
18.
Tsai KM, Telzer EH, Fuligni AJ. Continuity and discontinuity in perceptions of family relationships from adolescence to young adulthood. Child Dev. 2013;84(2):471–484. doi:10.1111/j.1467-8624.2012.01858.x.
19.
Zaborskis A, Kavaliauskiene A, Eriksson Ch, et al. Family Support as Smoking Prevention during Transition from Early to Late Adolescence: A Study in 42 Countries. Int J Environ Res Public Health. 2021;18(23): 12739. https://doi.org/10.3390/ijerph....
20.
World Health Organization. WHO Report on the Global Tobacco Epidemic, 2017: Monitoring Tobacco Use and Prevention Policie. Geneva: World Health Organization; 2017.
21.
Ngo A, Cheng KW, Chaloupka FJ, et al. The effect of MPOWER scores on cigarette smoking prevalence and consumption. Prev Med. 2017;105S:S10–S14. doi:10.1016/j.ypmed.2017.05.006.
22.
Levy DT, Li Y, Yuan Z. Impact of nations meeting the MPOWER targets between 2014 and 2016: An update. Tob Control. 2019;29(2). https://dx.doi.org/10.1136/tob....
23.
Wilson LM, Tang EA, Chander, G, et al. Impact of tobacco control interventions on smoking initiation, cessation, and prevalence: A systematic review. J Environ Public Health. 2012;2012:961724. doi:10.1155/2012/961724.
24.
Shang C, Chaloupka FJ, Gupta PC, et al. Association between tobacco prices and smoking onset: evidence from the TCP India Survey. Tob Control. 2019;28(Suppl 1):s3–s8. doi:10.1136/tobaccocontrol-2017-054178.
25.
Parks MJ, Patrick ME, Levy DT, et al. Tobacco Taxation and Its Prospective Impact on Disparities in Smoking Initiation and Progression Among Young Adults. J Adolesc Health. 2021;68(4):765–772. doi:10.1016/j.jadohealth.2020.08.031.
26.
Asare S, Stoklosa M, Drope J, et al. Effects of Prices on Youth Cigarette Smoking and Tobacco Use Initiation in Ghana and Nigeria. Int J Environ Res Public Health. 2019;6(17):3114. doi:10.3390/ijerph16173114.
27.
Ahmed MU, Pulok MH, Hashmi R, et al. Price and Income Elasticities of Cigarette Smoking Demand in Bangladesh: Evidence from Urban Adolescents and Young Adults. Nicotine Tob Res. 2022;24(6):826–833. doi:10.1093/ntr/ntab270.
28.
Vladisavljević M, Djukić M, Jovanović O, et al. How do prices of manufactured cigarettes and roll-your-own tobacco affect demand for these products? Tobacco price elasticity in Western Balkan countries. Tob Control 2022;0:1–8. doi:10.1136/tobaccocontrol-2021-056847.
29.
Diaz MC, Kierstead EC, Khatib BS, et al. Investigating the Impact of E-Cigarette Price and Tax on E-Cigarette Use Behavior. Am J Prev Med. 2023;S0749–3797(23)00019–3. doi:10.1016/j.amepre.2023.01.015. Online ahead of print.
30.
Summary results of the Global Youth Tobacco Survey in selected countries of the WHO European Region. Copenhagen: WHO Regional Office for Europe; 2020.
31.
Rao S, Aslam SK, Zaheer S, et al. Anti-smoking initiatives and current smoking among 19,643 adolescents in South Asia: findings from the global youth tobacco survey. Harm Reduct J. 2014;11:8.
32.
Aslam SK, Zaheer S, Rao S, et al. Prevalence and determinants of susceptibility to cigarette smoking among school students in Pakistan: secondary analysis of global youth tobacco survey. Subst Abuse Treat Prev Policy. 2014;9:1–10.
33.
Hock LK, Ghazali SM, Cheong KC, et al. Correlates of susceptibility to smoking among secondary school students in Kota Tinggi district, Johor, Malaysia. Asian Pac J Cancer Prev. 2013;14(11):6971–8. doi:10.7314/apjcp.2013.14.11.6971.
34.
Azagba S, Asbridge M. School connectedness and susceptibility to smoking among adolescents in Canada. Nicotine Tob Res. 2013;15(8): 1458–63.
35.
Veeranki SP, Mamudu HM, Anderson JL, et al. Worldwide never-smoking youth susceptibility to smoking. J Adolesc Health. 2014;54(2):144–50. doi:10.1016/j.jadohealth.2013.07.036.
36.
Nuno VL, Zhang Q, Harris RB, Wilkinson-Lee AM, Wilhelm MS. Smoking susceptibility among students followed from grade six to eight. Addict Behav. 2011;36(12):1261–6. doi:10.1016/j.addbeh.2011.07.041.
37.
Global Youth Tobacco Survey 2018. Montenegro, 2018. https://extranet.who.int/ncdsm... (access: 2023.05.01).
38.
2019 GYTS Fact Sheet Republic of Moldova. https://www.who.int/publicatio... (access: 2023.05.01).
40.
Global Youth Tobacco Survey 2018. San Marino, 2018. https://extranet.who.int/ncdsm... (access: 2023.05.01).
41.
Polańska K, Znyk M, Kaleta D. Susceptibility to tobacco use and associated factors among youth in five central and eastern European countries. BMC Public Health 2022;22:72. https://doi.org/10.1186/s12889....
42.
Ljaljević A, Mugoša B, Grbović E, Ćatić S. Montenegro 2018 country Report Global Youth Tobacco Survey (GYTS). Institute of Public Health of Montenegro: Podgorica; 2019.
43.
GTSSData. Centers for Disease Control and Prevention. https://www.cdc.gov/tobacco/gl... (access: 2023.05.01).
44.
Tobacco questions for surveys of youth (TQS-Youth): a subset of key questions from the Global Youth Tobacco Survey (GYTS). World Health Organization, 2019.
45.
Bafunno D, Catino A, Lamorgese V, et al. Tobacco control in Europe: a review of campaign strategies for teenagers and adults. Crit Rev Oncol Hematol. 2019;138:139–47. doi:10.1016/j.critrevonc.2019.01.022.
46.
Phetphum Ch, Prajongjeep A, Youngiam W, et al. Susceptibility to smoking and determinants among never-smoking high school students in Thailand. Tob Induc Dis. 2023;21:2. doi:10.18332/tid/156456.
47.
Yang X, Yan Z, Xu G, et al. How secondhand smoke exposure affects tobacco use and smoking susceptibility of adolescents: Sex and school differences. Tob Induc Dis. 2021;19:68. doi:10.18332/tid/140094.
48.
Lim KH, Lim HL, Teh CH, et al. Smoking among school-going adolescents in selected secondary schools in Peninsular Malaysia- findings from the Malaysian Adolescent Health Risk Behaviour (MyaHRB) study. Tob Induc Dis. 2017;15:9. doi:10.1186/s12971-016-0108-5.
49.
Peng S, Yu L, Yang T, et al. Susceptibility to smoking and determinants among medical students: A representative nationwide study in China. Tob Induc Dis. 2019;17:36. doi:10.18332/tid/106188.
50.
Zheng P, Berg CJ, Kegler MC, et al. Smoke-free homes and home exposure to secondhand smoke in Shanghai, China. Int J Environ Res Public Health. 2014;11(11):12015–28. doi:10.3390/ijerph111112015.
51.
Phetphum C, Noosorn N. Prevalence of secondhand smoke exposure at home and associated factors among middle school students in Northern Thailand. Tob Induc Dis. 2020;18:11. doi:10.18332/tid/117733.
52.
Rachiotis G, Barbouni A, Basagiannis A, et al. Prevalence and determinants of current cigarette smoking and secondhand smoking among Greek adolescents: the global youth tobacco survey (GYTS) 2013 study. BMJ Open. 2020;10(2):e034760.
53.
Khan JK, Raheem E, Daniel M. The prevalence and correlates of tobacco use among 7–9 th grade students in Bangladesh. Child Youth Serv Rev. 2019;104(C):1–1. Elsevier.
54.
Oztekin C, Batra M, Abdelsalam S, et al. Impact of individual, familial and parental factors on adolescent smoking in Turkey. Int J Environ Res Public Health. 2021;18(7):3740. doi:10.3390/ijerph18073740.
55.
Polańska K, Wojtysiak P, Bąk-Romaniszyn L, Kaleta D. Susceptibility to cigarette smoking among secondary and high school students from a socially disadvantaged rural area in Poland. Tob Induc Dis. 2016;14:28. doi:10.1186/s12971-016-0092-9.
56.
Huong LT, Vu NT, Dung NN, et al. Cigarette smoking among adolescents aged 13–15 in Viet Nam and correlates of current cigarette smoking: results from GYTS 2014 data. Asian Pac J Cancer Prev. 2016;17(S1):17–23. doi:10.7314/apjcp.2016.17.s1.17.
57.
Duko B, Yirdaw Melese Y, Ebrahim J. Determinants of cigarette smoking among adolescents in Ethiopia: a cross-sectional study. Tob Induc Dis. 2019;17:62. doi:10.18332/tid/110800.
58.
Mamudu HM, Veeranki SP, John RM. Tobacco use among school-going adolescents (11–17 years) in Ghana. Nicotine Tob Res. 2013;15(8):1355–64. doi:10.1093/ntr/nts269.
59.
Veeranki SP, Mamudu HM, John RM, et al. Prevalence and correlates of tobacco use among school-going adolescents in Madagascar. J Epidemiol Global Health. 2015;5(3):239–47. doi:10.1016/j.jegh.2014.12.005.
60.
Agaku IT, Alpert HR, Vardavas CI, et al. Use of smokeless tobacco and cigarettes among Nigerian youths: implications for tobacco control policies in Africa. J Subst Abus. 2014;19(1/2):75–80.
61.
Bobo FT, Thanasekaran P, Joice AJR, et al. Susceptibility to cigarette smoking and associated factors among high school students in western Ethiopia. BMC Res Notes. 2018;11(1):626. doi:10.1186/s13104-018-3734-6.
62.
Santano-Mogena E, Franco-Antonio C, Chimento-Díaz S, et al. Sci Rep. 2021;11(1):1988. doi:10.1038/s41598-021-81723-5.
63.
Palamar JJ, Zhou S, Sherman S, et al. Hookah use among U.S. high school seniors. Pediatrics. 2014;134(2):227–234. doi:10.1542/peds.2014-0538.
64.
El Kazdouh H, El-Ammari A, Bouftini S, et al. Adolescents, parents and teachers’ perceptions of risk and protective factors of substance use in Moroccan adolescents: a qualitative study. Subst Abuse Treat Prev Policy. 2018;13(1):1–12.
65.
Fithria F, Adlim M, Jannah SR, et al. Indonesian adolescents’ perspectives on smoking habits: a qualitative study. BMC Public Health. 2021;21(1):1–8.
66.
Talip T, Kifi N, Murang Z, et al. Smoking initiation and continuation a qualitative study among Bruneian male adolescents. Asian Pac J Cancer Prev. 2016;17(7):3533–40.
67.
Dereje N, Abazinab S, Girma A. Prevalence and predictors of cigarette smoking among adolescents of Ethiopia: school based cross-sectional survey. J Child Adolesc Behav. 2014;3:182. doi:10.4172/2375-4494.1000182.
68.
Roberts B, Stickley A, Gilmore A, et al. Knowledge of the health impacts of smoking and public attitudes towards tobacco control in the former Soviet Union. Tob Control. 2013;22(6):e12. doi:10.1136/tobaccocontrol-2011-050249.
69.
Long TK, Son PX, Giang KB, et al. Exposure to tobacco advertising and promotion among school children aged 13–15 in Vietnam – an overview from GYTS 2014. Asian Pac J Cancer Prev. 2016;17(S1):49–53. doi:10.7314/apjcp.2016.17.s1.49.
70.
Bogdanovica I, Szatkowski L, McNeill A, et al. Exposure to point-of-sale displays and changes in susceptibility to smoking: findings from a cohort study of school students. Addiction. 2015;110(4):693–702. doi:10.1111/add.12826.
71.
Pierce JP, Sargent JD, White MM, et al. Receptivity to tobacco advertising and susceptibility to tobacco products. Pediatrics. 2017;139(6):e20163353. doi:10.1542/peds.2016-3353.
72.
Shang C, Huang J, Li Q, et al. The Association between Point-of-Sale Advertising Bans and Youth Experimental Smoking: Findings from the Global Youth Tobacco Survey (GYTS). AIMS Public Health. 2015;2(4):832–43. doi:10.3934/publichealth.2015.4.832.
Udostępnij
ARTYKUŁ POWIĄZANY
Przetwarzamy dane osobowe zbierane podczas odwiedzania serwisu. Realizacja funkcji pozyskiwania informacji o użytkownikach i ich zachowaniu odbywa się poprzez dobrowolnie wprowadzone w formularzach informacje oraz zapisywanie w urządzeniach końcowych plików cookies (tzw. ciasteczka). Dane, w tym pliki cookies, wykorzystywane są w celu realizacji usług, zapewnienia wygodnego korzystania ze strony oraz w celu monitorowania ruchu zgodnie z Polityką prywatności. Dane są także zbierane i przetwarzane przez narzędzie Google Analytics (więcej).
Możesz zmienić ustawienia cookies w swojej przeglądarce. Ograniczenie stosowania plików cookies w konfiguracji przeglądarki może wpłynąć na niektóre funkcjonalności dostępne na stronie.
Możesz zmienić ustawienia cookies w swojej przeglądarce. Ograniczenie stosowania plików cookies w konfiguracji przeglądarki może wpłynąć na niektóre funkcjonalności dostępne na stronie.