Online first
Bieżący numer
Archiwum
O czasopiśmie
Polityka etyki publikacyjnej
System antyplagiatowy
Instrukcje dla Autorów
Instrukcje dla Recenzentów
Rada Redakcyjna
Komitet Redakcyjny
Recenzenci
Wszyscy recenzenci
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
Kontakt
Bazy indeksacyjne
Klauzula przetwarzania danych osobowych (RODO)
PRACA ORYGINALNA
Analiza porównawcza objawów depresji i jakości diety polskich wegetarian oraz osób spożywających mięso z wykorzystaniem Inwentarza Depresji Becka-II
1
Department of Biotechnology, Microbiology and Human Nutrition, University of Life Sciences in Lublin, Poland
2
Department of Psychology, Medical University of Lublin, Poland
3
Department of Food and Nutrition, Medical University of Lublin, Poland
Autor do korespondencji
Paulina Jedut
Uniwersytet Przyrodniczy w Lublinie, Katedra Biotechnologii, Mikrobiologii i Żywienia Człowieka, Skromna 8, 20-704 Lublin, Polska
Uniwersytet Przyrodniczy w Lublinie, Katedra Biotechnologii, Mikrobiologii i Żywienia Człowieka, Skromna 8, 20-704 Lublin, Polska
Med Og Nauk Zdr. 2023;29(3):214-223
SŁOWA KLUCZOWE
DZIEDZINY
STRESZCZENIE
Wprowadzenie i cel:
Jednym z czynników wpływających na rozwój i hamowanie objawów depresji jest żywność i składniki odżywcze. Celem pracy była analiza objawów depresji wśród polskich wegetarian i wszystkożerców za pomocą BDI-II oraz ocena jakości ich diety.
Materiał i metody:
W badaniu wzięło udział 50 wegetarianek i 50 kobiet spożywających mięso w wieku od 17 do 50 lat. Do analizy wykorzystano BDI-II, autorski kwestionariusz oraz dzienniczek żywieniowy.
Wyniki:
Analiza statystyczna nie wykazała istotnego związku między czasem trwania diety wegetariańskiej a występowaniem depresji. Nie stwierdzono korelacji pomiędzy suplementacją a pojawieniem się lub brakiem objawów depresji. Wegetarianki z objawami depresji dostarczały swojemu organizmowi odpowiednie ilości magnezu, przy czym wyniki te były istotne statystycznie. Niedobór witaminy B12 stwierdzono zarówno u wegetarianek z objawami depresji, jak i u tych bez takich objawów (p > 0,05). Spożycie kwasów tłuszczowych omega-3, tyrozyny, tryptofanu było wyższe wśród osób bez depresji zarówno w grupie wegetarianek, jak i wszystkożernych, jednak wyniki te nie były istotne statystycznie. Wegetarianki z objawami depresji piły więcej alkoholu (p > 0,05). Wegetarianki z objawami depresji i wszystkożerne bez objawów również spożywały najwięcej kofeiny (p > 0,05).
Wnioski:
Objawy depresyjne częściej występowały wśród wegetarianek. Z przeprowadzonej analizy wynika, że nie jest możliwe znalezienie przyczyny żywieniowej, która miałaby istotny wpływ na rozwój objawów depresyjnych. W badanej grupie wegetarianek odżywianie nie miało większego wpływu na wystąpienie lub brak objawów depresyjnych. Niemniej jednak istnieje potrzeba dodatkowych badań nad wpływem diety roślinnej na zdrowie psychiczne społeczności wegetariańskiej, nie tylko kobiet, ale także mężczyzn.
Jednym z czynników wpływających na rozwój i hamowanie objawów depresji jest żywność i składniki odżywcze. Celem pracy była analiza objawów depresji wśród polskich wegetarian i wszystkożerców za pomocą BDI-II oraz ocena jakości ich diety.
Materiał i metody:
W badaniu wzięło udział 50 wegetarianek i 50 kobiet spożywających mięso w wieku od 17 do 50 lat. Do analizy wykorzystano BDI-II, autorski kwestionariusz oraz dzienniczek żywieniowy.
Wyniki:
Analiza statystyczna nie wykazała istotnego związku między czasem trwania diety wegetariańskiej a występowaniem depresji. Nie stwierdzono korelacji pomiędzy suplementacją a pojawieniem się lub brakiem objawów depresji. Wegetarianki z objawami depresji dostarczały swojemu organizmowi odpowiednie ilości magnezu, przy czym wyniki te były istotne statystycznie. Niedobór witaminy B12 stwierdzono zarówno u wegetarianek z objawami depresji, jak i u tych bez takich objawów (p > 0,05). Spożycie kwasów tłuszczowych omega-3, tyrozyny, tryptofanu było wyższe wśród osób bez depresji zarówno w grupie wegetarianek, jak i wszystkożernych, jednak wyniki te nie były istotne statystycznie. Wegetarianki z objawami depresji piły więcej alkoholu (p > 0,05). Wegetarianki z objawami depresji i wszystkożerne bez objawów również spożywały najwięcej kofeiny (p > 0,05).
Wnioski:
Objawy depresyjne częściej występowały wśród wegetarianek. Z przeprowadzonej analizy wynika, że nie jest możliwe znalezienie przyczyny żywieniowej, która miałaby istotny wpływ na rozwój objawów depresyjnych. W badanej grupie wegetarianek odżywianie nie miało większego wpływu na wystąpienie lub brak objawów depresyjnych. Niemniej jednak istnieje potrzeba dodatkowych badań nad wpływem diety roślinnej na zdrowie psychiczne społeczności wegetariańskiej, nie tylko kobiet, ale także mężczyzn.
Introduction and objective:
Among the factors influencing the development and inhibition of depression symptoms are food and nutrients. The aim of the study was analysis of depression symptoms among vegetarians and omnivores in Poland using BDI-II and assessment of the quality of their diet.
Material and methods:
The study involved women, 50 vegetarians and 50 omnivores, aged 17–50. BDI-II, author›s questionnaire and nutritional diary were used for the analysis.
Results:
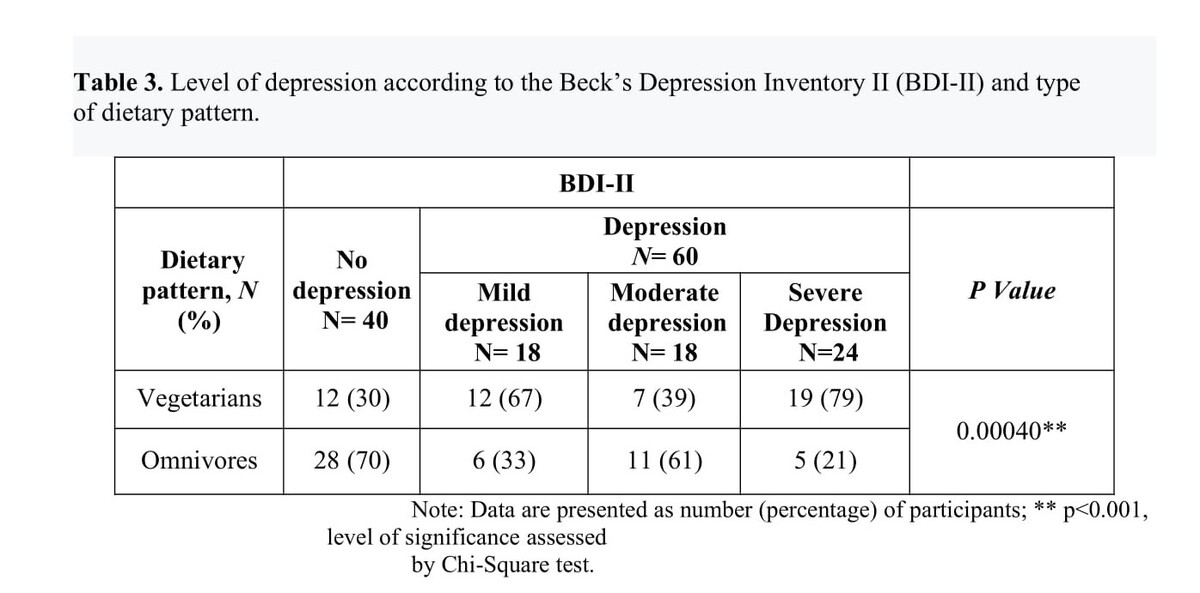
Statistical analysis showed no significant relationship between the duration of the vegetarian diet and the occurrence of depression. There was no correlation between supplementation and the appearance or absence of depression symptoms. Vegetarians with symptoms of depression provided adequate amounts of magnesium. The results were statistically significant. Vitamin B12 deficiency was found in vegetarians with and without depressive symptoms (p>0.05). The consumption of omega-3 fatty acids, tyrosine and tryptophan was higher among non-depressives among vegetarians and omnivores. These results were not statistically significant. Vegetarians with symptoms of depression consume more alcohol (p>0.05). Vegetarians with symptoms of depression and omnivores without symptoms also consumed the most caffeine (p>0.05).
Conclusions:
Depressive symptoms were more common among vegetarians. Analysis shows that it is impossible to find a nutritional cause that would have a significant impact on the development of depressive symptoms. In the studied group of vegetarians, nutrition was a insignificant factor in the presence or absence of depressive symptoms. Nevertheless, there is a need for additional research on the impact of a plantbased diet on the mental health of the vegetarian community, among both men and women.
Among the factors influencing the development and inhibition of depression symptoms are food and nutrients. The aim of the study was analysis of depression symptoms among vegetarians and omnivores in Poland using BDI-II and assessment of the quality of their diet.
Material and methods:
The study involved women, 50 vegetarians and 50 omnivores, aged 17–50. BDI-II, author›s questionnaire and nutritional diary were used for the analysis.
Results:
Statistical analysis showed no significant relationship between the duration of the vegetarian diet and the occurrence of depression. There was no correlation between supplementation and the appearance or absence of depression symptoms. Vegetarians with symptoms of depression provided adequate amounts of magnesium. The results were statistically significant. Vitamin B12 deficiency was found in vegetarians with and without depressive symptoms (p>0.05). The consumption of omega-3 fatty acids, tyrosine and tryptophan was higher among non-depressives among vegetarians and omnivores. These results were not statistically significant. Vegetarians with symptoms of depression consume more alcohol (p>0.05). Vegetarians with symptoms of depression and omnivores without symptoms also consumed the most caffeine (p>0.05).
Conclusions:
Depressive symptoms were more common among vegetarians. Analysis shows that it is impossible to find a nutritional cause that would have a significant impact on the development of depressive symptoms. In the studied group of vegetarians, nutrition was a insignificant factor in the presence or absence of depressive symptoms. Nevertheless, there is a need for additional research on the impact of a plantbased diet on the mental health of the vegetarian community, among both men and women.
Jedut P, Glibowski P, Styk W, Iłowiecka K. Comparative analysis of the depressive symptoms and diet quality between Polish vegetarians and
omnivores using Beck’s Depression Inventory-II. Med Og Nauk Zdr. 2023; 29(3): 214–223. doi: 10.26444/monz/170102
REFERENCJE (67)
1.
Światowy Dzień Walki z Depresją 2021 – Wojewódzka Stacja Sanitarno-Epidemiologiczna w Krakowie – Portal Gov.pl. Wojewódzka Stacja Sanitarno-Epidemiologiczna w Krakowie. Accessed May 14, 2023. https://www.gov.pl/web/wsse-kr....
2.
Kuehner C. Why is depression more common among women than among men? Lancet Psychiatry. 2017;4(2):146–158. doi:10.1016/S2215-0366(16)30263-2.
3.
Rondón Bernard JE. Depression: A Review of its Definition. MOJAMT. 2018;5(1). doi:10.15406/mojamt.2018.05.00082.
4.
Suchowiak S, Wszołek K, Suwalska J, et al. Screening for perinatal depression: a review of tools and barriers. Neuropsychiatria i Neuropsychologia/Neuropsychiatry and Neuropsychology. 2020;15(1):60–69. doi:10.5114/nan.2020.97402.
5.
Glibowski P, Misztal A. Wpływ diety na samopoczucie psychiczne. Bromatol Chem Toksykol. 2016;49(1):1–9.
6.
Sánchez-Villegas A, Delgado-Rodríguez M, Alonso A, et al. Association of the Mediterranean dietary pattern with the incidence of depression: the Seguimiento Universidad de Navarra/University of Navarra follow-up (SUN) cohort. Arch Gen Psychiatry. 2009;66(10):1090–1098. doi:10.1001/archgenpsychiatry.2009.129.
7.
Banyś K, Knopczyk M, Bobrowska-Korczak B. The importance of folic acid for the health of the human body. Farm Pol. 2020;76(2):79–87. doi:10.32383/farmpol/118863.
8.
Kühn S, Düzel S, Colzato L, et al. Food for thought: association between dietary tyrosine and cognitive performance in younger and older adults. Psychol Res. 2019;83(6):1097–1106. doi:10.1007/s00426-017-0957-4.
9.
Stępień A, Walecka-Kapica E, Błońska A, et al. Rola tryptofanu i serotoniny w patogenezie i leczeniu zespołu jelita nadwrażliwego. Fol Med Lodz. 2014;41(2):139–154.
10.
National Institutes of Health. Office of Dietary Supplements.: Vitamin B6: Health Professional Fact Sheet. 2022. Accessed May 14, 2023. http://ods. od.nih.gov/factsheets/vitaminb6/.
11.
National Institutes of Health. Office of Dietary Supplements.: Vitamin B12: Health Professional Fact Sheet. 2022. Accessed May 14, 2023. https://ods.od.nih.gov/factshe....
12.
Jedut P, Szwajgier D, Glibowski P, et al. Some Plant Food Products Present on the Polish Market Are a Source of Vitamin B12. Applied Sci. 2021;11(8):3601. doi:10.3390/app11083601.
13.
National Institutes of Health. Office of Dietary Supplements.: Folate: Health Professional Fact Sheet. 2022. Accessed May 14, 2023. https://ods.od.nih.gov/factshe....
14.
National Institutes of Health. Office of Dietary Supplements.: Zinc: Health Professional Fact Sheet. 2022. Accessed May 14, 2023. https://ods.od.nih.gov/factshe....
15.
National Institutes of Health. Office of Dietary Supplements.: Copper: Health Professional Fact Sheet. 2022. Accessed May 14, 2023. https://ods.od.nih.gov/factshe....
16.
National Institutes of Health. Office of Dietary Supplements.: Health Professional Fact Sheet. 2022. Accessed May 14, 2023. https://ods.od.nih.gov/factshe....
17.
National Institutes of Health. Office of Dietary Supplements.: Magnesium: Health Professional Fact Sheet. 2022. Accessed May 14, 2023. https://ods.od.nih.gov/factshe....
18.
National Institutes of Health. Office of Dietary Supplements. Omega-3 Fatty Acids: Health Professional Fact Sheet. 2023. Accessed May 14, 2023. https://ods.od.nih.gov/factshe....
19.
Aquili L. The Role of Tryptophan and Tyrosine in Executive Function and Reward Processing. Int J Tryptophan Res. 2020;13:1–13. doi:10.1177/1178646920964825.
20.
McNamara RK. Role of Omega-3 fatty acids in the etiology, treatment, and prevention of depression: Current status and future directions. J Nutr Intermed Metab. 2016;5:96–106. doi:10.1016/j.jnim.2016.04.004.
21.
Berkins S, Schiöth HB, Rukh G. Depression and Vegetarians: Association between Dietary Vitamin B6, B12 and Folate Intake and Global and Subcortical Brain Volumes. Nutr. 2021;13(6):1790. doi:10.3390/nu13061790.
22.
Li Z, Wang W, Xin X, Song X, Zhang D. Association of total zinc, iron, copper and selenium intakes with depression in the US adults. J Affect Disord. 2018;228:68–74. doi:10.1016/j.jad.2017.12.004.
23.
Pickering G, Mazur A, Trousselard M, et al. Magnesium Status and Stress: The Vicious Circle Concept Revisited. Nutr. 2020;12(12):3672. doi:10.3390/nu12123672.
24.
Martínez-González MA, Sánchez-Villegas A. Food patterns and the prevention of depression. Proc Nutr Soc. 2016;75(2):139–146. doi:10.1017/S0029665116000045.
25.
Dagnelie PC, Mariotti F. 1 – Vegetarian Diets: Definitions and Pitfalls in Interpreting Literature on Health Effects of Vegetarianism. In: Mariotti F, ed. Vegetarian and Plant-Based Diets in Health and Disease Prevention. Academic Press; 2017:3–10. doi:10.1016/B978-0-12-803968-7.00001-0.
26.
Marrone G, Guerriero C, Palazzetti D, et al. Vegan Diet Health Benefits in Metabolic Syndrome. Nutrients. 2021;13(3):817. doi:10.3390/nu13030817.
27.
Baş M, Karabudak E, Kiziltan G. Vegetarianism and eating disorders: association between eating attitudes and other psychological factors among Turkish adolescents. Appetite. 2005;44(3):309–315. doi:10.1016/j.appet.2005.02.002.
28.
Jin Y, Kandula NR, Kanaya AM, et al. Vegetarian diet is inversely associated with prevalence of depression in middle-older aged South Asians in the United States. Ethn Health. 2021;26(4):504–511. doi:10.1080/13557858.2019.1606166.
29.
Hibbeln JR, Northstone K, Evans J, et al. Vegetarian diets and depressive symptoms among men. J Affective Dis. 2018;225:13–17. doi:10.1016/j.jad.2017.07.051.
30.
Li Y, Lv MR, Wei YJ, et al. Dietary patterns and depression risk: A meta-analysis. Psychiatry Res. 2017;253:373–382. doi:10.1016/j.psychres.2017.04.020.
31.
Owen L, Corfe B. The role of diet and nutrition on mental health and wellbeing. Proc Nutr Soc. 2017;76(4):425–426. doi:10.1017/S0029665117001057.
32.
Beezhold B, Radnitz C, Rinne A, et al. Vegans report less stress and anxiety than omnivores. Nutr Neurosci. 2015;18(7):289–296. doi:10.1179/1476830514Y.0000000164.
33.
Askari M, Daneshzad E, Darooghegi Mofrad M, et al. Vegetarian diet and the risk of depression, anxiety, and stress symptoms: a systematic review and meta-analysis of observational studies. Crit Rev Food Sci Nutr. 2022;62(1):261–271. doi:10.1080/10408398.2020.1814991.
34.
Iguacel I, Huybrechts I, Moreno LA, et al. Vegetarianism and veganism compared with mental health and cognitive outcomes: a systematic review and meta-analysis. Nutr Rev. 2021;79(4):361–381. doi:10.1093/nutrit/nuaa030.
35.
Goldberg M, Carton M, Descatha A, et al. CONSTANCES: a general prospective population-based cohort for occupational and environmental epidemiology: cohort profile. Occup Environ Med. 2017;74(1):66–71. doi:10.1136/oemed-2016-103678.
36.
Lee MF, Eather R, Best T. Plant-based dietary quality and depressive symptoms in Australian vegans and vegetarians: a cross-sectional study. BMJ Nutr Prev Health. 2021;4(2):479–486. doi:10.1136/bmjnph-2021-000332.
37.
Kendall PC, Hollon SD, Beck AT, et al. Issues and recommendations regarding use of the Beck Depression Inventory. Cogn Ther Res. 1987;11(3):289–299. doi:10.1007/BF01186280.
38.
Zawadzki B, Popiel A, Pragłowska E. Charakterystyka psychometryczna polskiej adaptacji Kwestionariusza Depresji BDI-II Aarona T. Becka (Psychometric Properties of the Polish Version of the Aaron T. Beck’s Depression Inventory BDI-II). PSYCHOLOGIA – ETOLOGIA – GENETYKA. 2009;2009:71–95.
39.
Dietary reference values | EFSA. Published April 24, 2023. Accessed May 14, 2023. https://www.efsa.europa.eu/en/....
40.
Darimont T, Karavasiloglou N, Hysaj O, et al. Body weight and self-perception are associated with depression: Results from the National Health and Nutrition Examination Survey (NHANES) 2005–2016. J Affect Disord. 2020;274:929–934. doi:10.1016/j.jad.2020.05.130.
41.
Wiglusz MS, Landowski J, Michalak L, et al. Validation of the Polish version of the Beck Depression Inventory in patients with epilepsy. Epilepsy Behav. 2017;77:58–61. doi:10.1016/j.yebeh.2017.09.023.
42.
Bègue L, Shankland R. Is vegetarianism related to anxiety and depression? A cross-sectional survey in a French sample. Journal of Health, Population and Nutrition. 2022;41(1):18. doi:10.1186/s41043-022-00300-2.
43.
Stolińska H, Wolańska D. Analiza składu ciała kobiet na diecie tradycyjnej i wegetariańskiej. Żyw Czł Met. 2015;42(2):13–22.
44.
Grzelak T, Suliga K, Pelczyńska M, et al. Ocena częstości stosowania suplementów diety wśród wegetarian oraz osób odżywiających się tradycyjnie. Probl Hig Epidemiol. 2017;98(2):170–176.
45.
Schüpbach R, Wegmüller R, Berguerand C, et al. Micronutrient status and intake in omnivores, vegetarians and vegans in Switzerland. Eur J Nutr. 2017;56(1):283–293. doi:10.1007/s00394-015-1079-7.
46.
Tarleton EK, Littenberg B, MacLean CD, et al. Role of magnesium supplementation in the treatment of depression: A randomized clinical trial. PLoS One. 2017;12(6):e0180067. doi:10.1371/journal.pone.0180067.
47.
Kirkland AE, Sarlo GL, Holton KF. The Role of Magnesium in Neurological Disorders. Nutrients. 2018;10(6):730. doi:10.3390/nu10060730.
48.
Daneshzad E, Keshavarz SA, Qorbani M, et al. Dietary total antioxidant capacity and its association with sleep, stress, anxiety, and depression score: A cross-sectional study among diabetic women. Clin Nutr ESPEN. 2020;37:187–194. doi:10.1016/j.clnesp.2020.03.002.
49.
Sangle P, Sandhu O, Aftab Z, et al. Vitamin B12 Supplementation: Preventing Onset and Improving Prognosis of Depression. Cureus. 2020;12(10). doi:10.7759/cureus.11169.
50.
Wu Y, Zhang L, Li S, Zhang D. Associations of dietary vitamin B1, vitamin B2, vitamin B6, and vitamin B12 with the risk of depression: a systematic review and meta-analysis. Nutrition Rev. 2022;80(3):351–366. doi:10.1093/nutrit/nuab014.
51.
Todorov AA, Chumpalova-Tumbeva PG, Stoimenova-Popova MY, et al. Correlation between Depression and Anxiety and the Level of Vitamin B12 in Patients with Depression and Anxiety and Healthy Controls. J Biomedical Clin Res. 2017;10(2):140–145. doi:10.1515/jbcr-2017-0023.
52.
Klettner A, Perez E. 0166 The Role of Vitamin B12 Supplementation in the Association between Depression Symptoms and Daytime Sleepiness. Sleep. 2022;45(Supplement_1):A77. doi:10.1093/sleep/zsac079.164.
53.
Markun S, Gravestock I, Jäger L, et al. Effects of Vitamin B12 Supplementation on Cognitive Function, Depressive Symptoms, and Fatigue: A Systematic Review, Meta-Analysis, and Meta-Regression. Nutrients. 2021;13(3):923. doi:10.3390/nu13030923.
54.
Mehdi S, Manohar K, Shariff A, et al. Omega-3 Fatty Acids Supplementation in the Treatment of Depression: An Observational Study. J Personalized Med. 2023;13(2):224. doi:10.3390/jpm13020224.
55.
Healy-Stoffel M, Levant B. N-3 (Omega-3) Fatty Acids: Effects on Brain Dopamine Systems and Potential Role in the Etiology and Treatment of Neuropsychiatric Disorders. CNS Neurol Disord Drug Targets. 2018;17(3):216–232. doi:10.2174/1871527317666180412153612.
56.
Kopschina Feltes P, Doorduin J, Klein HC, et al. Anti-inflammatory treatment for major depressive disorder: implications for patients with an elevated immune profile and non-responders to standard antidepressant therapy. J Psychopharmacol. 2017;31(9):1149–1165. doi:10.1177/0269881117711708.
57.
Edwards R, Peet M, Shay J, et al. Depletion of docosahexaenoic acid in red blood cell membranes of depressive patients. Biochem Soc Trans. 1998;26(2):S142. doi:10.1042/bst026s142.
58.
Peet M, Murphy B, Shay J, et al. Depletion of omega-3 fatty acid levels in red blood cell membranes of depressive patients. Biol Psychiatry. 1998;43(5):315–319. doi:10.1016/s0006-3223(97)00206-0.
59.
Fontani G, Corradeschi F, Felici A, et al. Cognitive and physiological effects of Omega-3 polyunsaturated fatty acid supplementation in healthy subjects. Eur J Clin Invest. 2005;35(11):691–699. doi:10.1111/j.1365-2362.2005.01570.x.
60.
Rogers PJ, Appleton KM, Kessler D, et al. No effect of n-3 long-chain polyunsaturated fatty acid (EPA and DHA) supplementation on depressed mood and cognitive function: a randomised controlled trial. Br J Nutr. 2008;99(2):421–431. doi:10.1017/S0007114507801097.
61.
Peplińska-Miąskowska J, Wichowicz H, Waśkow M. Potencjalny wpływ wybranych składników diety na stan psychiczny: Neuropsychiatria Przegląd kliniczny. 2017;9(3):101–107.
62.
Maes M, Leonard BE, Myint AM, et al. The new “5-HT” hypothesis of depression: cell-mediated immune activation induces indoleamine 2,3-dioxygenase, which leads to lower plasma tryptophan and an increased synthesis of detrimental tryptophan catabolites (TRYCATs), both of which contribute to the onset of depression. Prog Neuropsychopharmacol Biol Psychiatry. 2011;35(3):702–721. doi:10.1016/j.pnpbp.2010.12.017.
63.
Lucas M, Mirzaei F, Pan A, et al. Coffee, caffeine, and risk of depression among women. Arch Intern Med. 2011;171(17):1571–1578. doi:10.1001/archinternmed.2011.393.
64.
Asil E, Yılmaz MV, Yardimci H. Effects of black tea consumption and caffeine intake on depression risk in black tea consumers. Afr Health Sci. 2021;21(2):858–865. doi:10.4314/ahs.v21i2.47.
65.
Guo X, Park Y, Freedman ND, et al. Sweetened beverages, coffee, and tea and depression risk among older US adults. PLoS One. 2014;9(4):e94715. doi:10.1371/journal.pone.0094715.
66.
McHugh RK, Weiss RD. Alcohol Use Disorder and Depressive Disorders. Alcohol Res. 2019;40(1):arcr.v40.1.01. doi:10.35946/arcr.v40.1.01.
67.
Rowicka M, Postek S, Zin-Sędek M. Wzory konsumpcji alkoholu w Polsce: Raport z badań kwestionariuszowych 2020 r. 2021: 12–20.
Udostępnij
ARTYKUŁ POWIĄZANY
Przetwarzamy dane osobowe zbierane podczas odwiedzania serwisu. Realizacja funkcji pozyskiwania informacji o użytkownikach i ich zachowaniu odbywa się poprzez dobrowolnie wprowadzone w formularzach informacje oraz zapisywanie w urządzeniach końcowych plików cookies (tzw. ciasteczka). Dane, w tym pliki cookies, wykorzystywane są w celu realizacji usług, zapewnienia wygodnego korzystania ze strony oraz w celu monitorowania ruchu zgodnie z Polityką prywatności. Dane są także zbierane i przetwarzane przez narzędzie Google Analytics (więcej).
Możesz zmienić ustawienia cookies w swojej przeglądarce. Ograniczenie stosowania plików cookies w konfiguracji przeglądarki może wpłynąć na niektóre funkcjonalności dostępne na stronie.
Możesz zmienić ustawienia cookies w swojej przeglądarce. Ograniczenie stosowania plików cookies w konfiguracji przeglądarki może wpłynąć na niektóre funkcjonalności dostępne na stronie.