Online first
Bieżący numer
Archiwum
O czasopiśmie
Polityka etyki publikacyjnej
System antyplagiatowy
Instrukcje dla Autorów
Instrukcje dla Recenzentów
Rada Redakcyjna
Komitet Redakcyjny
Recenzenci
Wszyscy recenzenci
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
Kontakt
Bazy indeksacyjne
Klauzula przetwarzania danych osobowych (RODO)
PRACA ORYGINALNA
Wpływ poszczególnych parametrów stylu życia na subiektywną ocenę jakości snu u polskich dorosłych
1
Institute of Health Sciences, Medical College of Rzeszow University, Rzeszów, Poland
Autor do korespondencji
Mateusz Jan Szałajko
Institute of Health Sciences, Medical College of Rzeszow University, 35-959 Rzeszów, Poland
Institute of Health Sciences, Medical College of Rzeszow University, 35-959 Rzeszów, Poland
Med Og Nauk Zdr. 2024;30(1):49-55
SŁOWA KLUCZOWE
DZIEDZINY
STRESZCZENIE
Wprowadzenie i cel:
Zaburzenia snu są obecnie uważane za jedne z najczęstszych dolegliwości wśród dorosłych na całym świecie. Istnieje wiele czynników mogących mieć wpływ na zaburzenia snu, są to m.in. nieprawidłowa higiena snu, przewlekły stres, stosowanie używek czy nieprawidłowa dieta. Celem badania było poznanie związku między nawykami żywieniowymi a subiektywną oceną jakości snu u osób dorosłych.
Materiał i metody:
W badaniu wzięło udział 520 losowo wybranych dorosłych Polaków: 388 kobiet i 132 mężczyzn. Do gromadzenia danych wykorzystano metodę badania diagnostycznego z użyciem kwestionariusza składającego się z 3 części: metryczki, kwestionariusza oceny jakości snu i kwestionariusza oceny jakości żywienia.
Wyniki:
Tylko 29,8% respondentów było zadowolonych ze snu. Zdecydowana większość badanych deklarowała przeciętną jakość snu – 81,2%. Statystycznie istotne korelacje ze wskaźnikiem jakości snu występowały tylko dla częstotliwości spożywania napojów energetycznych (p = 0,0051) i napojów słodzonych (p = 0,0429). Wraz ze wzrostem częstotliwości spożywania tych produktów wzrastał wskaźnik jakości snu, a tym samym jakość snu badanych ulegała pogorszeniu.
Wnioski:
Na jakość snu mogą wpływać negatywnie zarówno czynniki żywieniowe, takie jak: nieregularne posiłki, niskie spożycie warzyw i owoców, picie napojów słodzonych i napojów zawierających kofeinę, jak i pozostałe czynniki stylu życia, tj. niska aktywność fizyczna czy palenie papierosów. Kluczowe dla zbadania związku między nawykami żywieniowymi a subiektywną podejście do problemu bezsenności, uwzględniające szeroko pojęty styl życia i higienę snu.
Zaburzenia snu są obecnie uważane za jedne z najczęstszych dolegliwości wśród dorosłych na całym świecie. Istnieje wiele czynników mogących mieć wpływ na zaburzenia snu, są to m.in. nieprawidłowa higiena snu, przewlekły stres, stosowanie używek czy nieprawidłowa dieta. Celem badania było poznanie związku między nawykami żywieniowymi a subiektywną oceną jakości snu u osób dorosłych.
Materiał i metody:
W badaniu wzięło udział 520 losowo wybranych dorosłych Polaków: 388 kobiet i 132 mężczyzn. Do gromadzenia danych wykorzystano metodę badania diagnostycznego z użyciem kwestionariusza składającego się z 3 części: metryczki, kwestionariusza oceny jakości snu i kwestionariusza oceny jakości żywienia.
Wyniki:
Tylko 29,8% respondentów było zadowolonych ze snu. Zdecydowana większość badanych deklarowała przeciętną jakość snu – 81,2%. Statystycznie istotne korelacje ze wskaźnikiem jakości snu występowały tylko dla częstotliwości spożywania napojów energetycznych (p = 0,0051) i napojów słodzonych (p = 0,0429). Wraz ze wzrostem częstotliwości spożywania tych produktów wzrastał wskaźnik jakości snu, a tym samym jakość snu badanych ulegała pogorszeniu.
Wnioski:
Na jakość snu mogą wpływać negatywnie zarówno czynniki żywieniowe, takie jak: nieregularne posiłki, niskie spożycie warzyw i owoców, picie napojów słodzonych i napojów zawierających kofeinę, jak i pozostałe czynniki stylu życia, tj. niska aktywność fizyczna czy palenie papierosów. Kluczowe dla zbadania związku między nawykami żywieniowymi a subiektywną podejście do problemu bezsenności, uwzględniające szeroko pojęty styl życia i higienę snu.
Introduction and objective:
Sleep disorders are now considered to be one of the most common ailments among adults worldwide. There are many factors that can affect sleep disorders, including poor sleep hygiene, chronic stress, the use of stimulants or improper diet. The aim of the study is to investigate the relationship between eating habits and subjective sleep quality assessment in adults.
Material and methods:
The study involved 520 randomly selected Polish adults – 388 women and 132 men. A diagnostic survey method was used in the data collection using a questionnaire consisting of 3 parts: metric, Sleep Quality Assessment Questionnaire and Dietary Quality Assessment Questionnaire.
Results:
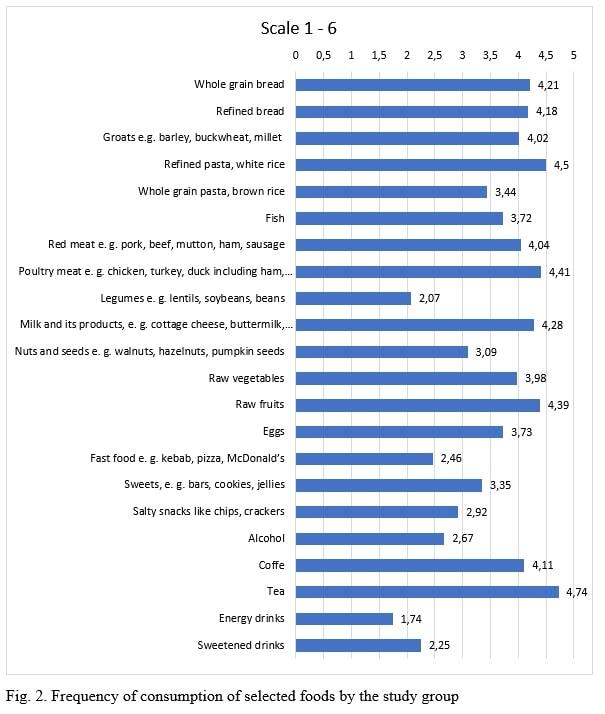
Only 29 (8%) of respondents were satisfied with their sleep. The vast majority declared normal sleep quality – 81 (2%). Statistically significant correlations with the sleep quality index occurred only for frequency of consumption of energy drinks (p=0.0051) and sweetened drinks (p=0.0429). As the frequency of consumption of these products increased, the sleep quality index increased, and thus the sleep quality of the subjects deteriorated.
Conclusions:
Nutritional factors, such as irregular meals, low intake of fruit and vegetables, sugary and caffeinecontaining beverages, as well as other lifestyle factors, such as low physical activity and smoking, may also affect sleep quality. Most important is a holistic approach to the problem of insomnia, taking into account a broadly understood lifestyle and sleep hygiene.
Sleep disorders are now considered to be one of the most common ailments among adults worldwide. There are many factors that can affect sleep disorders, including poor sleep hygiene, chronic stress, the use of stimulants or improper diet. The aim of the study is to investigate the relationship between eating habits and subjective sleep quality assessment in adults.
Material and methods:
The study involved 520 randomly selected Polish adults – 388 women and 132 men. A diagnostic survey method was used in the data collection using a questionnaire consisting of 3 parts: metric, Sleep Quality Assessment Questionnaire and Dietary Quality Assessment Questionnaire.
Results:
Only 29 (8%) of respondents were satisfied with their sleep. The vast majority declared normal sleep quality – 81 (2%). Statistically significant correlations with the sleep quality index occurred only for frequency of consumption of energy drinks (p=0.0051) and sweetened drinks (p=0.0429). As the frequency of consumption of these products increased, the sleep quality index increased, and thus the sleep quality of the subjects deteriorated.
Conclusions:
Nutritional factors, such as irregular meals, low intake of fruit and vegetables, sugary and caffeinecontaining beverages, as well as other lifestyle factors, such as low physical activity and smoking, may also affect sleep quality. Most important is a holistic approach to the problem of insomnia, taking into account a broadly understood lifestyle and sleep hygiene.
Szałajko MJ, Dereń K. The influence of individual lifestyle parameters on subjective sleep quality assessment in Polish adults. Med Og Nauk
Zdr. 2024; 30(1): 49–55. doi: 10.26444/monz/185729
REFERENCJE (26)
1.
Sykut A, Ślusarska B, Jędrzejkiewicz, et al. Sleep disorders as a common social problem – selected determinants and health consequences. Pielęgniarstwo XXI wieku. 2017;16(2):59. https://doi.org/10.1515/pielxx....
2.
Irwin M. Sleep and inflammation: partners in sickness and in health. Nat Rev Immunol. 2019;19:702–715. https://doi.org/10.1038/s41577....
3.
So-Ngern A, Chirakalwasan N, Saetung S, et al. Effects of Two-Week Sleep Extension on Glucose Metabolism in Chronically Sleep-Deprived Individuals. J Clin Sleep Med. 2019;15(5):711–718. https://doi.org/10.5664/jcsm.7....
4.
Bubu OM, Brannick M, Mortimer J, et al. Sleep, Cognitive impairment, and Alzheimer's disease: A Systematic Review and Meta-Analysis. Sleep. 2017;40(1). doi:10.1093/sleep/zsw032.
5.
Garbarino S, Lanteri P, Bragazzi NL, et al. Role of sleep deprivation in immune-related disease risk and outcomes. Commun Biol. 2021;4(1):1304. doi:10.1038/s42003-021-02825-4.
6.
Yang CL, Schnepp J, Tucker RM. Increased Hunger, Food Cravings, Food Reward, and Portion Size Selection after Sleep Curtailment in Women Without Obesity. Nutrients. 2019;11(3):663. https://doi.org/10.3390/nu1103....
7.
Stony Brook Medicine. Sleep deprivation in teens linked to poor dietary choices. https://www.sciencedaily.com/r... (access: 2022.11.14).
8.
Dashti HS, Scheer FA, Jacques PF, et al. Short sleep duration and dietary intake: epidemiologic evidence, mechanisms, and health implications. Adv Nutr. 2015;6(6):648–59. https://doi.org/10.3945/an.115....
9.
Kasperczyk J, Jośko J. The analysis of factors responsible for poor sleep quality in Silesian Medical School students. Hygeia Public Health. 2012;47(2):191–195.
10.
Taillard J, Gronfier C, Bioulac S, Philip P, Sagaspe P. Sleep in Normal Aging, Homeostatic and Circadian Regulation and Vulnerability to Sleep Deprivation. Brain Sci. 2021;11(8):1003. https://doi.org/10.3390/brains....
11.
Morin CM, Jarrin DC. Epidemiology of Insomnia: Prevalence, Course, Risk Factors, and Public Health Burden. Sleep Med Clin. 2022;17(2):173–191. doi:10.1016/j.jsmc.2022.03.003. Epub 2022 Apr 23. PMID: 35659072.
12.
Shaib F. Epidemiology of Sleep Disorders in Women. Sleep Disorders in Women. Current Clinical Neurology. 2020;9–15. https://doi.org/10.1007/978-3-....
13.
Peuhkuri K, Sihvola N, Korpela R. Diet promotes sleep duration and quality. Nutr Res. 2012;32(5):309–19. https://doi.org/10.1016/j.nutr....
14.
St-Onge MP, Mikic A, Pietrolungo CE. Effects of Diet on Sleep Quality. Adv Nutr. 2016;7(5):938–49. https://doi.org/10.3945/an.116....
15.
Rodak K, Kokot I, Kratz EM. Caffeine as a Factor Influencing the Functioning of the Human Body-Friend or Foe? Nutrients. 2021;13(9):3088. https://doi.org/10.3390/nu1309....
16.
dePaula J, Farah A. Caffeine Consumption through Coffee: Content in the Beverage, Metabolism, Health Benefits and Risks. Beverages. 2019;5(2):37. https://doi.org/10.3390/bevera....
17.
Doherty R, Madigan S, Warrington G, Ellis J. Sleep and Nutrition Interactions: Implications for Athletes. Nutrients. 2019;11(4):822. https://doi.org/10.3390/nu1104....
18.
Krajewska O, Skrypnik K, Kręgielska-Narożna M et al. Influence of sleep duration and quality on anthropometric, metabolic and general physical and mental health parameters. Metabolic Disorders Forum. 2017;8(2):47–54.
19.
Yilmaz D, Tanrikulu F, Dikmen Y. Research on Sleep Quality and the Factors Affecting the Sleep Quality of the Nursing Students. Curr Health Sci J. 2017;43(1):20–24. doi:10.12865/CHSJ.43.01.03.
20.
Min C, Kim HJ, Park IS, et al. The association between sleep duration, sleep quality, and food consumption in adolescents: A cross-sectional study using the Korea Youth Risk Behavior Web-based Survey. BMJ Open. 2018;8(7):e022848. doi:10.1136/bmjopen-2018-022848.
21.
Yasuda J, Yoshizaki T, Yamamoto K, et al. Association of Frequency of Milk or Dairy Product Consumption with Subjective Sleep Quality during Training Periods in Japanese Elite Athletes: A Cross-Sectional Study. J Nutr Sci Vitaminol (Tokyo). 2019;65(2):177–183. doi:10.3177/jnsv.65.177. PMID: 31061287.
22.
Tambalis KD, Panagiotakos DB, Psarra G, et al. Association between fast-food consumption and lifestyle characteristics in Greek children and adolescents; results from the EYZHN (National Action for Children's Health) programme. Public Health Nutr. 2018; 21(18): 3386–3394. doi:10.1017/S1368980018002707.
23.
Hong SA, Peltzer K. Dietary behaviour, psychological well-being and mental distress among adolescents in Korea. Child Adolesc Psychiatry Ment Health. 2017;11:56. doi:10.1186/s13034-017-0194-z.
24.
Dube N, Khan K, Loehr S, et al. The use of entertainment and communication technologies before sleep could affect sleep and weight status: a population-based study among children. Int J Behav Nutr Phys. 2017;14:97. https://doi.org/10.1186/s12966....
25.
Wang F, Boros S. The effect of physical activity on sleep quality: a systematic review, European Journal of Physiotherapy. 2021;23(1):11–18. doi:10.1080/21679169.2019.1623314.
26.
Liao Y, Xie L, Chen X, et al. Sleep quality in cigarette smokers and nonsmokers: findings from the general population in central China. BMC Public Health. 2019;19:808. https://doi.org/10.1186/s12889....
Udostępnij
ARTYKUŁ POWIĄZANY
Przetwarzamy dane osobowe zbierane podczas odwiedzania serwisu. Realizacja funkcji pozyskiwania informacji o użytkownikach i ich zachowaniu odbywa się poprzez dobrowolnie wprowadzone w formularzach informacje oraz zapisywanie w urządzeniach końcowych plików cookies (tzw. ciasteczka). Dane, w tym pliki cookies, wykorzystywane są w celu realizacji usług, zapewnienia wygodnego korzystania ze strony oraz w celu monitorowania ruchu zgodnie z Polityką prywatności. Dane są także zbierane i przetwarzane przez narzędzie Google Analytics (więcej).
Możesz zmienić ustawienia cookies w swojej przeglądarce. Ograniczenie stosowania plików cookies w konfiguracji przeglądarki może wpłynąć na niektóre funkcjonalności dostępne na stronie.
Możesz zmienić ustawienia cookies w swojej przeglądarce. Ograniczenie stosowania plików cookies w konfiguracji przeglądarki może wpłynąć na niektóre funkcjonalności dostępne na stronie.