Online first
Bieżący numer
Archiwum
O czasopiśmie
Polityka etyki publikacyjnej
System antyplagiatowy
Instrukcje dla Autorów
Instrukcje dla Recenzentów
Rada Redakcyjna
Komitet Redakcyjny
Recenzenci
Wszyscy recenzenci
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
Kontakt
Bazy indeksacyjne
Klauzula przetwarzania danych osobowych (RODO)
PRACA PRZEGLĄDOWA
Depresja poporodowa u mężczyzn – rzadko rozumiany częsty problem
1
Students’ Scientific Circle at the Department of Applied Psychology, Medical University, Lublin, Poland
2
Department of Applied Psychology, Medical University, Lublin, Poland
Autor do korespondencji
Magdalena Leśniewska
Studenckie Koło Naukowe przy Zakładzie Psychologii Stosowanej, Uniwersytet Medyczny w Lublinie, ul.Chodźki 7, 20-093, Lublin, Polska
Studenckie Koło Naukowe przy Zakładzie Psychologii Stosowanej, Uniwersytet Medyczny w Lublinie, ul.Chodźki 7, 20-093, Lublin, Polska
Med Og Nauk Zdr. 2021;27(3):248-251
SŁOWA KLUCZOWE
DZIEDZINY
STRESZCZENIE
Wprowadzenie i cel:
Depresję poporodową definiuje się jako pojawienie się epizodu depresyjnego w okresie po porodzie, ze szczytem występowania między 3. a 6. miesiącem od rozwiązania. Szacuje się, że obecnie problem ten dotyczy 1 na 10 ojców, a mimo to większość badań skupia się jedynie na depresji poporodowej matek.
Cel pracy:
Celem badania była analiza doniesień nauko-wych nt. depresji poporodowej u mężczyzn (PPPD – paternal postpartum depression). W tym celu dokonano przeglądu dostępnego piśmiennictwa na temat „Poporodowa depre-sja wśród mężczyzn”, korzystając w tym celu z baz danych: Scopus, PubMed oraz OVIDMedline.
Opis stanu wiedzy:
Kwestionariuszem stosowanym w diag-nostyce PPPD jest Edinburgh Postnatal Depression Scale, który jest wykorzystywany jako test skriningowy w kierunku depresji poporodowej występującej u matek, ale znalazł także zasto-sowanie w przypadku ojców.
Wyniki:
Ojcowie dostrzegali problem braku edukacji w zakresie opieki zdrowotnej w odniesieniu do ich potrzeb w okresie okołoporodowym oraz niedobór wsparcia specjalistów. Zaburzony stan psychiczny ojca uniemożliwia mu wzięcie pełnej odpowiedzialności za rodzinę i obciąża psychicznie matkę. Jednocześnie zła relacja partnerska jest czynnikiem ryzyka PPPD. Depresja poporodowa u mężczyzn stanowi niebezpieczeństwo dla ich nowo narodzonych dzieci, znajdujących się w okresie ich rozwoju, kiedy to są szczególnie wrażliwe
Podsumowanie:
Ojcowie powinni być poddawani testom scriningowym celem wczesnego wykrywania PPPD i pod-jęcia interwencji. PPPD jest zaburzeniem, w odniesieniu do którego brakuje odpowiednich narzędzi diagnostycznych. Uświadamianie społeczeństwa na temat PPPD jest ważne, ponieważ ojcowie są szczególnie narażeni na PPPD, chcąc spełnić tradycyjne oczekiwania i podejmować nowoczesne zadania związane z ojcostwem
Depresję poporodową definiuje się jako pojawienie się epizodu depresyjnego w okresie po porodzie, ze szczytem występowania między 3. a 6. miesiącem od rozwiązania. Szacuje się, że obecnie problem ten dotyczy 1 na 10 ojców, a mimo to większość badań skupia się jedynie na depresji poporodowej matek.
Cel pracy:
Celem badania była analiza doniesień nauko-wych nt. depresji poporodowej u mężczyzn (PPPD – paternal postpartum depression). W tym celu dokonano przeglądu dostępnego piśmiennictwa na temat „Poporodowa depre-sja wśród mężczyzn”, korzystając w tym celu z baz danych: Scopus, PubMed oraz OVIDMedline.
Opis stanu wiedzy:
Kwestionariuszem stosowanym w diag-nostyce PPPD jest Edinburgh Postnatal Depression Scale, który jest wykorzystywany jako test skriningowy w kierunku depresji poporodowej występującej u matek, ale znalazł także zasto-sowanie w przypadku ojców.
Wyniki:
Ojcowie dostrzegali problem braku edukacji w zakresie opieki zdrowotnej w odniesieniu do ich potrzeb w okresie okołoporodowym oraz niedobór wsparcia specjalistów. Zaburzony stan psychiczny ojca uniemożliwia mu wzięcie pełnej odpowiedzialności za rodzinę i obciąża psychicznie matkę. Jednocześnie zła relacja partnerska jest czynnikiem ryzyka PPPD. Depresja poporodowa u mężczyzn stanowi niebezpieczeństwo dla ich nowo narodzonych dzieci, znajdujących się w okresie ich rozwoju, kiedy to są szczególnie wrażliwe
Podsumowanie:
Ojcowie powinni być poddawani testom scriningowym celem wczesnego wykrywania PPPD i pod-jęcia interwencji. PPPD jest zaburzeniem, w odniesieniu do którego brakuje odpowiednich narzędzi diagnostycznych. Uświadamianie społeczeństwa na temat PPPD jest ważne, ponieważ ojcowie są szczególnie narażeni na PPPD, chcąc spełnić tradycyjne oczekiwania i podejmować nowoczesne zadania związane z ojcostwem
Introduction:
Postpartum depression (PPPD) is defined as the occurrence of a depressive episode in the postpartum period, with a peak incidence between 3–6 months. It is estimated that 1 in 10 fathers are currently affected, yet most research focuses only on postpartum depression in mothers.
Objective:
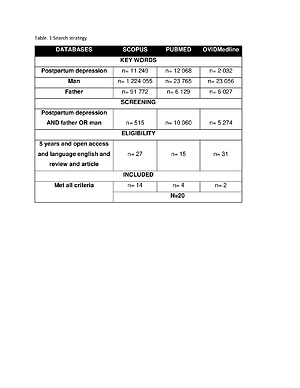
The aim of the study was to analyze scientific reports on paternal postpartum depression in men. The available literature on ‘postpartum depression among men’ was reviewed based on the Scopus, PubMed and OVIDMedline databases.
Brief description of the state of knowledge:
The questionnaire useiIn the diagnosis of PPPD is the Edinburgh Postnatal Depression Scale (EPDS), a screening test for postnatal depression occurring in mothers, but it has also found application in fathers
Results:
Fathers perceived a lack of perinatal health care education in relation to their needs and a shortage of specialist support. The father’s disturbed mental state prevents him from taking full responsibility for the family and places a mental strain on the mother. At the same time, a poor partner relationship is a risk factor for PPPD. Paternal PPD is a danger to newborn children who are at a critical stage of their development
Conclusions:
Fathers should be screened for early detection of PPPD and intervention in a disorder that lacks appropriate diagnostic tools. Public awareness of PPPD is important because fathers are particularly vulnerable, and can be lacking in meeting traditional expectations and modern fatherhood tasks.
Postpartum depression (PPPD) is defined as the occurrence of a depressive episode in the postpartum period, with a peak incidence between 3–6 months. It is estimated that 1 in 10 fathers are currently affected, yet most research focuses only on postpartum depression in mothers.
Objective:
The aim of the study was to analyze scientific reports on paternal postpartum depression in men. The available literature on ‘postpartum depression among men’ was reviewed based on the Scopus, PubMed and OVIDMedline databases.
Brief description of the state of knowledge:
The questionnaire useiIn the diagnosis of PPPD is the Edinburgh Postnatal Depression Scale (EPDS), a screening test for postnatal depression occurring in mothers, but it has also found application in fathers
Results:
Fathers perceived a lack of perinatal health care education in relation to their needs and a shortage of specialist support. The father’s disturbed mental state prevents him from taking full responsibility for the family and places a mental strain on the mother. At the same time, a poor partner relationship is a risk factor for PPPD. Paternal PPD is a danger to newborn children who are at a critical stage of their development
Conclusions:
Fathers should be screened for early detection of PPPD and intervention in a disorder that lacks appropriate diagnostic tools. Public awareness of PPPD is important because fathers are particularly vulnerable, and can be lacking in meeting traditional expectations and modern fatherhood tasks.
REFERENCJE (24)
1.
Scarff JR. Postpartum Depression in Men. Innov Clin Neurosci. 2019; 16(5–6): 11–14. PMID: 31440396; PMCID: PMC6659987.
2.
Soliday E, McCluskey-Fawcett K, O'Brien M. Postpartum affect and depressive symptoms in mothers and fathers. Am J Orthopsychiatry. 1999; 69(1): 30–8. https://doi.org/10.1037/h00803....
3.
Koch S, De Pascalis L, Vivian F, Meurer Renner A, Murray L, Arteche A. Effects of male postpartum depression on father-infant interaction: The mediating role of face processing. Infant Ment Health J. 2019; 40(2): 263–276. https://doi.org/10.1002/imhj.2....
4.
Johansson M, Benderix Y, Svensson I. Mothers' and fathers' lived experiences of postpartum depression and parental stress after childbirth: a qualitative study. Int J Qual Stud Health Well-being. 2020; 15(1): 1722564. https://doi.org/10.1080/174826....
5.
Leach LS, Poyser C, Cooklin AR, Giallo R. Prevalence and course of anxiety disorders (and symptom levels) in men across the perinatal period: A systematic review. J Affect Disord. 2016; 190: 675–686. https://doi.org/10.1016/j.jad.....
6.
Cameron EE, Sedov ID, Tomfohr-Madsen LM. Prevalence of paternal depression in pregnancy and the postpartum: An updated meta-analysis. J Affect Disord. 2016; 206: 189–203. https://doi.org/10.1016/j.jad.....
7.
Albicker J, Hölzel LP, Bengel J, Domschke K, Kriston L, Schiele MA, Frank F. Prevalence, symptomatology, risk factors and healthcare services utilization regarding paternal depression in Germany: study protocol of a controlled cross-sectional epidemiological study. BMC Psychiatry. 2019; 19(1): 289. https://doi.org/10.1186/s12888....
8.
Cameron EE, Hunter D, Sedov ID, Tomfohr-Madsen LM. What do dads want? Treatment preferences for paternal postpartum depression. J Affect Disord. 2017; 215: 62–70. https://doi.org/10.1016/j.jad.....
9.
Francisca Pérez C, Anthea Catalán, Alyson Morales, Antonia Quinlan, Diego Riquelme, Javiera Navarro, Camila Valdés.Assessment of Postpartum Depression in a Group of Chilean Parents. Journal of Men's Health. 2018. 14(2); 56–64. https://doi.org/10.22374/1875-....
10.
Shaheen NA, AlAtiq Y, Thomas A, Alanazi HA, AlZahrani ZE, Younis SAR, Hussein MA. Paternal Postnatal Depression Among Fathers of Newborn in Saudi Arabia. Am J Mens Health. 2019; 13(1): 1557988319831219. ht t ps://doi.org /10.1177/1557988319831219.
11.
Loscalzo Y, Giannini M, Contena B, Gori A, Benvenuti P. The Edinburgh Postnatal Depression Scale for Fathers: A contribution to the validation for an Italian sample. Gen Hosp Psychiatry. 2015; 37(3): 251–6. https://doi.org/10.1016/j.genh....
12.
Mayers A, Hambidge S, Bryant O, et al. Supporting women who develop poor postnatal mental health: what support do fathers receive to support their partner and their own mental health?. BMC Pregnancy Childbirth 20; 359(2020). https://doi.org/10.1186/s12884....
13.
Hughes C, Foley S, Devine RT, Ribner A, Kyriakou L, Boddington L, Holmes EA; NewFAMS team Creators/Copyright Holders; NewFAMS team Contributors. Worrying in the wings? Negative emotional birth memories in mothers and fathers show similar associations with perinatal mood disturbance and delivery mode. Arch Womens Ment Health. 2020; 23(3): 371–377. https://doi.org/10.1007/s00737....
14.
Psouni E, Agebjörn J, Linder H. Symptoms of depression in Swedish fathers in the postnatal period and development of a screening tool. Scand J Psychol. 2017; 58(6): 485–496. https://doi.org/10.1111/sjop.1....
15.
Schipper-Kochems S, Fehm T, Bizjak G, Fleitmann AK, Balan P, Hagenbeck C, Schäfer R, Franz M. Postpartum Depressive Disorder – Psychosomatic Aspects. Geburtshilfe Frauenheilkd. 2019; 79(4): 375–381. https://doi.org/10.1055/a-0759....
16.
Letourneau N, Leung B, Ntanda H, Dewey D, Deane AJ, Giesbrecht GF; APrON Team. Maternal and paternal perinatal depressive symptoms associate with 2- and 3-year-old children's behaviour: findings from the APrON longitudinal study. BMC Pediatr. 2019; 19(1): 435. https://doi.org/10.1186/s12887....
17.
Gutierrez-Galve L, Stein A, Hanington L, Heron J, Ramchandani P. Paternal depression in the postnatal period and child development: mediators and moderators. Pediatrics. 2015; 135(2): e339–47. https://doi.org/10.1542/peds.2....
18.
Paulson JF, Bazemore SD. Prenatal and postpartum depression in fathers and its association with maternal depression: a meta-analysis. JAMA. 2010; 303(19): 1961–9. https://doi.org/10.1001/jama.2....
19.
Cao H, Yuan X, Fine M, Zhou N, Fang X. Neuroticism and Marital Satisfaction During the Early Years of Chinese Marriage: The Mediating Roles of Marital Attribution and Aggression. Fam Process. 2019; 58(2): 478– 495. ht t ps://doi.org /10.1111/fa mp.12356.
20.
Kiviruusu O, Pietikäinen JT, Kylliäinen A, Pölkki P, Saarenpää-Heikkilä O, Marttunen M, Paunio T, Paavonen EJ. Trajectories of mothers' and fathers' depressive symptoms from pregnancy to 24 months postpartum. J Affect Disord. 2020; 260: 629–637. https://doi.org/10.1016/j.jad.....
21.
Bamishigbin ON Jr, Wilson DK, Abshire DA, Mejia-Lancheros C, Dunkel Schetter C. Father Involvement in Infant Parenting in an Ethnically Diverse Community Sample: Predicting Paternal Depressive Symptoms. Front Psychiatry. 2020; 11: 578688. https://doi.org/10.3389/fpsyt.....
22.
Edward KL, Giandinoto JA, Stephenson J, Mills C, Mcfarland J, Castle DJ. Self- screening using the Edinburgh postnatal depression scale for mothers and fathers to initiate early help seeking behaviours. Arch Psychiatr Nurs. 2019; 33(4): 421–427. https://doi.org/10.1002/da.204....
23.
Wells MB, Massoudi P, Bergström M. Swedish child health nurses treat fathers more equally in 2014 than 2004, but mothers remain their primary focus. Acta Paediatr. 2017; 106(8): 1302–1308. https://doi.org /10.1111/apa.13898.
24.
Missler M, Beijers R, Denissen J, van Straten A. Effectiveness of a psycho-educational intervention to prevent postpartum parental distress and enhance infant well-being: study protocol of a randomized controlled trial. Trials. 2018; 19(1): 4. https://doi.org/10.1186/s13063....
Udostępnij
ARTYKUŁ POWIĄZANY
Przetwarzamy dane osobowe zbierane podczas odwiedzania serwisu. Realizacja funkcji pozyskiwania informacji o użytkownikach i ich zachowaniu odbywa się poprzez dobrowolnie wprowadzone w formularzach informacje oraz zapisywanie w urządzeniach końcowych plików cookies (tzw. ciasteczka). Dane, w tym pliki cookies, wykorzystywane są w celu realizacji usług, zapewnienia wygodnego korzystania ze strony oraz w celu monitorowania ruchu zgodnie z Polityką prywatności. Dane są także zbierane i przetwarzane przez narzędzie Google Analytics (więcej).
Możesz zmienić ustawienia cookies w swojej przeglądarce. Ograniczenie stosowania plików cookies w konfiguracji przeglądarki może wpłynąć na niektóre funkcjonalności dostępne na stronie.
Możesz zmienić ustawienia cookies w swojej przeglądarce. Ograniczenie stosowania plików cookies w konfiguracji przeglądarki może wpłynąć na niektóre funkcjonalności dostępne na stronie.