RESEARCH PAPER
Communication between doctors and nurses with patients as one of the indicators of the quality of provided medical services"
1
Zakład Medycyny Społecznej, Wydział Nauk o Zdrowiu, Uniwersytet Medyczny w Łodzi, Polska
2
Department of Social Medicine, Faculty of Health Sciences, Medical University of Lodz, Polska
Corresponding author
Anna Agnieszka Warczyńska
Zakład Medycyny Społecznej, Wydział Nauk o Zdrowiu, Uniwersytet Medyczny w Łodzi, ul. Żeligowskiego 7/9, 90-752 Łódź, Polska
Zakład Medycyny Społecznej, Wydział Nauk o Zdrowiu, Uniwersytet Medyczny w Łodzi, ul. Żeligowskiego 7/9, 90-752 Łódź, Polska
Med Og Nauk Zdr. 2025;31(2):126-131
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
The way of communication with patients affects both the quality of healthcare services and patient satisfaction. Empathy, clear explanation of procedures, and active listening encourage adherence to medical recommendations and enhance therapy safety. The aim of this study was to assess the role of doctor-patient and nursepatient communication in selected primary healthcare centres, and to determine to what extent the quality of communication serves as a measure of service quality.
Material and methods:
The study was conducted from March 2019 – March 2020 in three randomly selected primary healthcare centres. The PASAT POZ1 questionnaire and an author-designed survey were used. Anonymous data from 1,118 completed questionnaires were analyzed using SPSS Statistics 29.0.
Results:
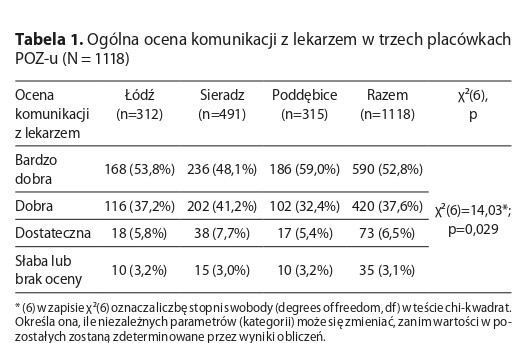
The study confirmed the predominant effect of communication with doctors and nurses on patient trust and satisfaction. In the Poddębice centre, 67% of assessments of medical staff communication were rated as ‘very good’” Spearman’s rank correlations (r_s=0.62–0.68) indicated the key role of empathy and health education, whereas long queues for doctor appointments (r_s=–0.35) significantly lowered patient satisfaction. It is recommended to intensify pro-health education and develop soft skills among medical staff in primary healthcare centres.
Conclusions:
Proper communication by doctors and nurses promotes better adherence to recommendations and increases trust in the medical team. Variations in the level of communication observed in the studied centres indicate the need for systematic training in interpersonal skills and optimization of appointment times. The findings confirm that communication should be a priority measure in healthcare management and its improvement may exert a significant effect on patient satisfaction with treatment.
The way of communication with patients affects both the quality of healthcare services and patient satisfaction. Empathy, clear explanation of procedures, and active listening encourage adherence to medical recommendations and enhance therapy safety. The aim of this study was to assess the role of doctor-patient and nursepatient communication in selected primary healthcare centres, and to determine to what extent the quality of communication serves as a measure of service quality.
Material and methods:
The study was conducted from March 2019 – March 2020 in three randomly selected primary healthcare centres. The PASAT POZ1 questionnaire and an author-designed survey were used. Anonymous data from 1,118 completed questionnaires were analyzed using SPSS Statistics 29.0.
Results:
The study confirmed the predominant effect of communication with doctors and nurses on patient trust and satisfaction. In the Poddębice centre, 67% of assessments of medical staff communication were rated as ‘very good’” Spearman’s rank correlations (r_s=0.62–0.68) indicated the key role of empathy and health education, whereas long queues for doctor appointments (r_s=–0.35) significantly lowered patient satisfaction. It is recommended to intensify pro-health education and develop soft skills among medical staff in primary healthcare centres.
Conclusions:
Proper communication by doctors and nurses promotes better adherence to recommendations and increases trust in the medical team. Variations in the level of communication observed in the studied centres indicate the need for systematic training in interpersonal skills and optimization of appointment times. The findings confirm that communication should be a priority measure in healthcare management and its improvement may exert a significant effect on patient satisfaction with treatment.
REFERENCES (22)
1.
Kamiński K. Zarządzanie jakością w podmiotach leczniczych. Wydawnictwo ABC; 2018. s. 25–26.
2.
Włodarczyk C. System opieki zdrowotnej w Polsce. Perspektywa pacjenta. Wydawnictwo PZWL; 2017. s. 114–117.
3.
Smith M, Clarke A. Patient-centred communication in primary care: a systematic review. J Prim Health Care. 2019;12(3):15–27.
4.
Kowalski T, Nowak M. Znaczenie komunikacji w pracy zespołów medycznych. Med Prakt. 2019;3(2):15–28.
5.
Smith JA, Taylor P. Patient-centered communication in modern healthcare. Int J Health Sci. 2020;12(4):112–115.
6.
World Health Organization. Communication in healthcare: a policy brief. WHO; 2016. s. 25–29.
7.
Miller L, Grant R. Improving interpersonal skills of medical staff. BMC Med Educ. 2017;17(1):48–52.
8.
James B, Froelicher E. Communication patterns in clinical nursing. Clin Nurs Res. 2021;30(3):217–223.
9.
Kwiatkowska A, Dróżdż W. Znaczenie empatii w kontaktach lekarz–pacjent. Zdrow Publiczne. 2016;126(2):35–40.
10.
Andersson H, Petersson K. Challenges of nurse-patient communication in multicultural settings. Nurs Reflect Pract. 2018;9(1):6–12.
11.
Chen Y, Li L. The role of nonverbal cues in doctor-patient interactions. J Health Commun. 2020;25(2):72–80.
12.
Centrum Monitorowania Jakości w Ochronie Zdrowia. Standardy akredytacyjne dla podstawowej opieki zdrowotnej. CMJ; 2019. s. 33–34.
13.
Warchoł K, Duda T. Współpraca pielęgniarek i lekarzy a poziom bezpieczeństwa pacjentów. Pielęg Pol. 2016;4(62):97–105. s. 98–100.
14.
Novak M, Piechota R. Standardy komunikacji w pielęgniarstwie – przegląd literatury. Pielęg XXI w. 2017;16(2):15–21.
15.
Johnson F, Tickle S. Nurses as patient educators in chronic disease management. J Adv Nurs. 2016;72(2):243–247.
16.
Marques P, Santos R. Emotional strain in nursing practice: significance of communication. Eur J Nurs Sci. 2021;14(1):298–307.
17.
Górska E, Przybylski J. Wpływ komunikacji personelu medycznego na proces powrotu do zdrowia pacjentów. Zdrow Publiczne i Zarządzanie. 2019;17(1):94–101.
18.
Kaczmarek J, Waszkiewicz A, Walczak B, et al. Komunikacja lekarz–pacjent w aspekcie satysfakcji z leczenia w POZ. Fam Med Prim Care Rev. 2018;20(2):233–239.
19.
Gajewski P, Szczeklik A. Interna Szczeklika. Kraków: Medycyna Praktyczna; 2021. s. 99–102.
20.
Edgman-Levitan S, Schoenbaum SC. Patient experience and satisfaction: essential but not the whole picture. Health Aff. 2020;39(2):23–31.
21.
Johnson F, Tickle S. Nurses as patient educators in chronic disease management. J Adv Nurs. 2016;72(2):244–246.
22.
Roux A, Jefferson B. Measuring patient adherence through communication metrics. Patient Prefer Adherence. 2019;13:10–15.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.