Online first
Bieżący numer
Archiwum
O czasopiśmie
Polityka etyki publikacyjnej
System antyplagiatowy
Instrukcje dla Autorów
Instrukcje dla Recenzentów
Rada Redakcyjna
Komitet Redakcyjny
Recenzenci
Wszyscy recenzenci
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
Kontakt
Bazy indeksacyjne
Klauzula przetwarzania danych osobowych (RODO)
PRACA PRZEGLĄDOWA
Szczepienia donosowe przeciwko grypie, krztuścowi i COVID-19: skuteczność kliniczna, wyzwania immunologiczne oraz rozwój metod prewencji chorób układu oddechowego
1
Lifestyle Medicine Scientific Student Group, Department of Biochemical Science, Pomeranian Medical University, Szczecin, Poland
2
Department of Biochemical Science, Pomeranian Medical University, Szczecin, Poland
Autor do korespondencji
Joanna Walczyńska
Studenckie Koło Naukowe Medycyny Stylu Życia przy Zakładzie Badań Biochemicznych Pomorskiego Uniwersytetu Medycznego w Szczecinie, Polska, Pomorski Uniwersytet Medyczny w Szczecinie, Polska
Studenckie Koło Naukowe Medycyny Stylu Życia przy Zakładzie Badań Biochemicznych Pomorskiego Uniwersytetu Medycznego w Szczecinie, Polska, Pomorski Uniwersytet Medyczny w Szczecinie, Polska
Med Og Nauk Zdr. 2025;31(4):211-218
SŁOWA KLUCZOWE
DZIEDZINY
STRESZCZENIE
Wprowadzenie i cel:
Choroby układu oddechowego, takie jak grypa, COVID-19 czy krztusiec, stanowią istotne zagrożenie dla zdrowia publicznego, szczególnie dla osób z grup ryzyka, takich jak osoby starsze i przewlekle chore. Celem niniejszego artykułu jest ocena potencjału szczepionek donosowych jako nowoczesnej, bezpiecznej i obiecującej alternatywy dla klasycznych metod immunizacji, zwłaszcza w kontekście zapobiegania rozprzestrzenianiu się chorób zakaźnych.
Metody przeglądu:
Przegląd literatury oparto na bazach PubMed i Google Scholar (do 31 grudnia 2024 roku), bez ograniczeń co do daty publikacji. Wykorzystano hasła: „szczepienie przeciwko krztuścowi”, „szczepienie przeciwko COVID-19” oraz „szczepienie przeciwko grypie”. Uwzględniono badania na modelach zwierzęcych i ludzkich dotyczące skuteczności szczepień donosowych
Opis stanu wiedzy:
Donosowe preparaty przeciwko grypie, krztuścowi i COVID-19 wykazują duży potencjał. Zawarte w nich substancje hydrożelowe mogą wydłużać obecność antygenu w jamie nosowej i wspomagać rozwój pamięci immunologicznej. BPZE1 to szczepionka przeciw krztuścowi, która cechuje się dobrą tolerancją i skutecznością. Wskazuje się również, że połączenie szczepień donosowych z ogólnoustrojowymi może nasilać odpowiedź odpornościową.
Podsumowanie:
Szczepionki donosowe są skuteczne w indukowaniu śluzówkowej i ogólnoustrojowej odpowiedzi immunologicznej przeciwko krztuścowi, grypie i SARS-CoV-2. Obecne wyniki sugerują, że mogą one stać się ważnym narzędziem zapobiegania chorobom układu oddechowego i wymagają przeprowadzenia dalszych badań klinicznych.
Choroby układu oddechowego, takie jak grypa, COVID-19 czy krztusiec, stanowią istotne zagrożenie dla zdrowia publicznego, szczególnie dla osób z grup ryzyka, takich jak osoby starsze i przewlekle chore. Celem niniejszego artykułu jest ocena potencjału szczepionek donosowych jako nowoczesnej, bezpiecznej i obiecującej alternatywy dla klasycznych metod immunizacji, zwłaszcza w kontekście zapobiegania rozprzestrzenianiu się chorób zakaźnych.
Metody przeglądu:
Przegląd literatury oparto na bazach PubMed i Google Scholar (do 31 grudnia 2024 roku), bez ograniczeń co do daty publikacji. Wykorzystano hasła: „szczepienie przeciwko krztuścowi”, „szczepienie przeciwko COVID-19” oraz „szczepienie przeciwko grypie”. Uwzględniono badania na modelach zwierzęcych i ludzkich dotyczące skuteczności szczepień donosowych
Opis stanu wiedzy:
Donosowe preparaty przeciwko grypie, krztuścowi i COVID-19 wykazują duży potencjał. Zawarte w nich substancje hydrożelowe mogą wydłużać obecność antygenu w jamie nosowej i wspomagać rozwój pamięci immunologicznej. BPZE1 to szczepionka przeciw krztuścowi, która cechuje się dobrą tolerancją i skutecznością. Wskazuje się również, że połączenie szczepień donosowych z ogólnoustrojowymi może nasilać odpowiedź odpornościową.
Podsumowanie:
Szczepionki donosowe są skuteczne w indukowaniu śluzówkowej i ogólnoustrojowej odpowiedzi immunologicznej przeciwko krztuścowi, grypie i SARS-CoV-2. Obecne wyniki sugerują, że mogą one stać się ważnym narzędziem zapobiegania chorobom układu oddechowego i wymagają przeprowadzenia dalszych badań klinicznych.
Introduction and objective:
Respiratory diseases, such as influenza, COVID-19 and pertussis, pose a significant public health threat, especially among at-risk groups such as the elderly and chronically ill. The aim of the study is to assess the potential of intranasal vaccines as a modern, safe and promising alternative to classical immunization methods, especially in the context of preventing the spread of infectious diseases.
Review methods:
A literature review was performed based on PubMed and Google Scholar databases (up to 31 December 2024), with no restrictions on publication date. The search terms used were: ‘pertussis vaccination’, ‘COVID-19 vaccination’, and ‘influenza vaccination’. Studies in animal and human models on the efficacy of intranasal vaccination were included.
Brief description of the state of knowledge:
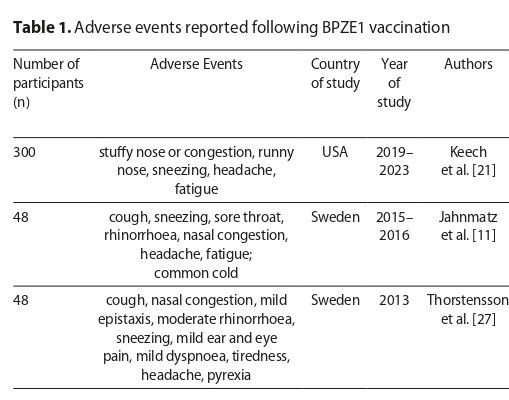
Intranasal preparations against influenza, pertussis and COVID-19 show great potential. The use of hydrogel substances can prolong the presence of the antigen in the nasal cavity, promoting the development of durable immunity. BPZE1 is a pertussis vaccine with good tolerability and efficacy in clinical trials. It has also been shown that the combination of intranasal and systemic vaccines can enhance the immune response.
Summary:
Intranasal vaccines are effective in inducing mucosal and systemic immune responses against pertussis, influenza and SARS-CoV-2. The results obtained suggest that they may become an important tool for the prevention of respiratory diseases and further clinical trials are required.
Respiratory diseases, such as influenza, COVID-19 and pertussis, pose a significant public health threat, especially among at-risk groups such as the elderly and chronically ill. The aim of the study is to assess the potential of intranasal vaccines as a modern, safe and promising alternative to classical immunization methods, especially in the context of preventing the spread of infectious diseases.
Review methods:
A literature review was performed based on PubMed and Google Scholar databases (up to 31 December 2024), with no restrictions on publication date. The search terms used were: ‘pertussis vaccination’, ‘COVID-19 vaccination’, and ‘influenza vaccination’. Studies in animal and human models on the efficacy of intranasal vaccination were included.
Brief description of the state of knowledge:
Intranasal preparations against influenza, pertussis and COVID-19 show great potential. The use of hydrogel substances can prolong the presence of the antigen in the nasal cavity, promoting the development of durable immunity. BPZE1 is a pertussis vaccine with good tolerability and efficacy in clinical trials. It has also been shown that the combination of intranasal and systemic vaccines can enhance the immune response.
Summary:
Intranasal vaccines are effective in inducing mucosal and systemic immune responses against pertussis, influenza and SARS-CoV-2. The results obtained suggest that they may become an important tool for the prevention of respiratory diseases and further clinical trials are required.
Kiedrowska K, Pawlicka AA, Walczyńska J, Skonieczna-Żydecka K. Intranasal Vaccination Against Influenza, Pertussis, and COVID-19: Clinical
Efficacy, Immunological Challenges, and Development of Prevention of Respiratory Diseases. Med Og Nauk Zdr. 2025;31(4):211–218.
doi:10.26444/monz/213322
REFERENCJE (51)
1.
Karaś R, Barszczewski K, Biadasiewicz M, Kulik H, Lepich T. Edward Jenner (1749–1823), the pioneer of vaccinology. On the bicentenary of his death. Farm Współcz. 2023;16:91–7.
2.
Plotkin S. History of vaccination. Proc Natl Acad Sci U S A. 2014 Aug 26;111(34):12283–7. Epub 2014 Aug 18.
3.
Francis T, Magil TP. Vaccination of human subjects with virus of human influenza. Proc Soc Exp Biol Med. 1936;33:604–6.
4.
Proud PC, Tsitoura D, Watson RJ, Chua BY, Aram MJ, Bewley KR, et al. Prophylactic intranasal administration of a TLR2/6 agonist reduces upper respiratory tract viral shedding in a SARS-CoV-2 challenge ferret model. EBioMedicine. 2021;63:103153. Epub 2020 Dec 3.
7.
Mbayei SA, Faulkner A, Miner C, Edge K, Cruz V, Peña SA, et al. Severe pertussis infections in the United States, 2011–2015. Clin Infect Dis. 2019 Jul 2;69(2):218–26.
8.
de Graaf H, Ibrahim M, Hill AR, Gbesemete D, Vaughan AT, Gorringe A, et al. Controlled human infection with Bordetella pertussis induces asymptomatic, immunizing colonization. Clin Infect Dis. 2020 Jul 11;71(2):403–11.
9.
Locht C. Pertussis: acellular, whole-cell, new vaccines, what to choose? Expert Rev Vaccines. 2016;15(6):671–3. Epub 2016 Mar 21.
10.
Galeas-Pena M, Hirsch A, Kuang E, Hoffmann J, Gellings P, Brown JB, et al. A novel outer membrane vesicle adjuvant improves vaccine protection against Bordetella pertussis. NPJ Vaccines. 2024 Oct 16;9(1):190.
11.
Jahnmatz M, Richert L, Al-Tawil N, Storsaeter J, Colin C, Bauduin C, et al. Safety and immunogenicity of the live attenuated intranasal pertussis vaccine BPZE1: a phase 1b, double-blind, randomised, placebo-controlled dose-escalation study. Lancet Infect Dis. 2020;20(11):1290–301. Epub 2020 Jul 17.
12.
Saleh A, Qamar S, Tekin A, Singh R, Kashyap R. Vaccine Development Throughout History. Cureus. 2021 Jul 26;13(7):e16635.
13.
Ankomah AA, Moa A, Chughtai AA. The long road of pandemic vaccine development to rollout: a systematic review on the lessons learnt from the 2009 H1N1 influenza pandemic. Am J Infect Control. 2022;50(7):735–42. Epub 2022 Feb 4.
14.
Brisse M, Vrba SM, Kirk N, Liang Y, Ly H. Emerging concepts and technologies in vaccine development. Front Immunol. 2020 Sep 30;11:583077.
15.
Johns Hopkins University. Coronavirus Resource Center. COVID-19 dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University. 2020.
16.
Williamson EJ, Walker AJ, Bhaskaran K, Bacon S, Bates C, Morton CE, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584(7821):430–6. Epub 2020 Jul 8.
17.
Polack FP, Thomas SJ, Kitchin N, Absalon J, Gurtman A, Lockhart S, et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N Engl J Med. 2020 Dec 31;383(27):2603–15. Epub 2020 Dec 10.
18.
Tang J, Zeng C, Cox TM, Li C, Son YM, Cheon IS, et al. Respiratory mucosal immunity against SARS-CoV-2 after mRNA vaccination. Sci Immunol. 2022 Oct 28;7(76):eadd4853. Epub 2022 Oct 21.
19.
Bedford JG, Caminschi I, Wakim LM. Intranasal delivery of a chitosanhydrogel vaccine generates nasal tissue resident memory CD8+ T cells that are protective against influenza virus infection. Vaccines. 2020 Oct 1;8(4):572.
20.
Turner PJ, Abdulla AF, Cole ME, Javan RR, Gould V, O’Driscoll ME, et al. Differences in nasal immunoglobulin A responses to influenza vaccine strains after live attenuated influenza vaccine immunization in children. Clin Exp Immunol. 2020;199(2):109–18. Epub 2019 Nov 15.
21.
Keech C, Miller VE, Rizzardi B, Hoyle C, Pryor MJ, Ferrand J, et al. Immunogenicity and safety of BPZE1, an intranasal live attenuated pertussis vaccine, versus tetanus-diphtheria-acellular pertussis vaccine: a randomised, double-blind, phase 2b trial. Lancet. 2023 Mar 11;401(10379):843–55.
22.
Feunou PF, Ismaili J, Debrie AS, Huot L, Hot D, Raze D, et al. Genetic stability of the live attenuated Bordetella pertussis vaccine candidate BPZE1. Vaccine. 2008 Oct 23;26(45):5722–7. Epub 2008 Aug 30.
23.
Cherry JD, Feigin RD. Textbook of pediatric infectious diseases. Philadelphia: WB Saunders Company; 1998.
24.
Shields MD, Bush A, Everard ML, McKenzie S, Primhak R. BTS guidelines: Recommendations for the assessment and management of cough in children. Thorax. 2008;63(Suppl 3):iii1–15. Epub 2007 Sep 28.
25.
Centers for Disease Control and Prevention (CDC). Recommended antimicrobial agents for the treatment and postexposure prophylaxis of pertussis: 2005 CDC Guidelines. MMWR Recomm Rep. 2005;54(RR-14):1–16. Available from: https://www.cdc.gov/mmwr/previ....
26.
Solans L, Debrie AS, Borkner L, Aguiló N, Thiriard A, Coutte L, et al. IL-17-dependent SIgA-mediated protection against nasal Bordetella pertussis infection by live attenuated BPZE1 vaccine. Mucosal Immunol. 2018;11(6):1753–62. Epub 2018 Aug 16.
27.
Thorstensson R, Trollfors B, Al-Tawil N, Jahnmatz M, Bergström
J, Ljungman M, et al. A phase I clinical study of a live attenuated Bordetella pertussis vaccine—BPZE1; a single centre, double-blind, placebo-controlled, dose-escalating study of BPZE1 given intranasally to healthy adult male volunteers. PLoS One. 2014 Jan 8;9(1):e83449.
28.
Lin A, Apostolovic D, Jahnmatz M, Liang F, Ols S, Tecleab T, et al. Live attenuated pertussis vaccine BPZE1 induces a broad antibody response in humans. J Clin Invest. 2020 May 1;130(5):2332–46.
29.
Belcher T, Ait-Yahia S, Solans L, Debrie AS, Cauchi S, Tsicopoulos A, et al. Live attenuated pertussis vaccine for prevention and treatment of allergic airway inflammation in mice. NPJ Vaccines. 2022 Jun 23;7(1):66.
30.
Jahnmatz M, Amu S, Ljungman M, Wehlin L, Chiodi F, Mielcarek N, et al. B-cell responses after intranasal vaccination with the novel attenuated Bordetella pertussis vaccine strain BPZE1 in a randomized phase I clinical trial. Vaccine. 2014 Jun 5;32(27):3350–6. Epub 2014 Apr 29.
31.
Ellis JA, Gow SP, Waldner CL, Shields S, Wappel S, Bowers A, et al. Comparative efficacy of intranasal and oral vaccines against Bordetella bronchiseptica in dogs. Vet J. 2016;212:71–7. Epub 2016 Apr 12.
32.
Aibani N, Patel P, Buchanan R, Strom S, Wasan KM, Hancock REW, et al. Assessing the in vivo effectiveness of cationic lipid nanoparticles with a triple adjuvant for intranasal vaccination against the respiratory pathogen Bordetella pertussis. Mol Pharm. 2022 Jun 6;19(6):1814–24. Epub 2022 Mar 18.
33.
Sherman AC, Mehta A, Dickert NW, Anderson EJ, Rouphael N. The future of flu: a review of the human challenge model and systems biology for advancement of influenza vaccinology. Front Cell Infect Microbiol. 2019 Apr 17;9:107.
34.
Minozzi S, Lytras T, Gianola S, Gonzalez-Lorenzo M, Castellini G, Galli C, et al. Comparative efficacy and safety of vaccines to prevent seasonal influenza: a systematic review and network meta-analysis. EClinicalMedicine. 2022 Mar 22;46:101331.
35.
Wood JM, Weir JP. Standardisation of inactivated influenza vaccines— learning from history. Influenza Other Respir Viruses. 2018;12(2):195–201. Epub 2018 Feb 2.
36.
European Medicines Agency. 2013. Fluenz Tetra – Public Assessment Report. Available online: https://www.ema.europa.eu/en/m... (accessed on 4 Septemper 2025).
37.
Cole ME, Kundu R, Abdulla AF, Andrews N, Hoschler K, Southern J, et al. Pre-existing influenza-specific nasal IgA or nasal viral infection does not affect live attenuated influenza vaccine immunogenicity in children. Clin Exp Immunol. 2021;204(1):125–33.
38.
Thwaites RS, Uruchurtu ASS, Negri VA, Cole ME, Singh N, Poshai N, et al. Early mucosal events promote distinct mucosal and systemic antibody responses to live attenuated influenza vaccine. Nat Commun.2023 Dec 5;14(1):8053.
39.
Jeong H, Lee CS, Lee J, Lee J, Hwang HS, Lee M, et al. Hemagglutinin nanoparticulate vaccine with controlled photochemical immunomodulation for pathogenic influenza-specific immunity. Adv Sci. 2021;8(23):e2100118. Epub 2021 Oct 24.
40.
World Health Organization. Influenza (Seasonal). 2025. Available online: https://www.who.int/en/news-ro...) (accessed on 4 Septemper 2025).
41.
Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020 Apr 16;181(2):271–80.e8. Epub 2020 Mar 5.
42.
Baden LR, El Sahly HM, Essink B, Kotloff K, Frey S, Novak R, et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N Engl J Med. 2021 Feb 4;384:403–16. Epub 2020 Dec 30.
43.
European Medicines Agency. Vaxzevria. https://www.ema.europa.eu/en/m... (accessed on 4 Septemper 2025).
44.
European Medicines Agency. Jcovden. https://www.ema.europa.eu/en/m... (accessed on 4 Septemper 2025).
45.
Novavax. U.S. FDA approves BLA for Novavax’s COVID-19 vaccine. 2025 May 19. https://ir.novavax.com/press-r... (accessed on 4 Septemper 2025).
46.
Hồ NT, Hughes SG, Ta VT, Phan LT, Đỗ Q, Nguyễn TV, et al. Safety, immunogenicity and efficacy of the self-amplifying mRNA ARCT-154 COVID-19 vaccine: pooled phase 1, 2, 3a and 3b randomized, controlled trials. Nat Commun. 2024 May 14;15(1):4081.
47.
Chen J, Wang P, Yuan L, Zhang L, Zhang L, Zhao H, et al. A live attenuated virus-based intranasal COVID-19 vaccine provides rapid, prolonged, and broad protection against SARS-CoV-2. Sci Bull. 2022 Jul 15;67(13):1372–87. Epub 2022 May 26.
48.
Zhou R, Wang P, Wong YC, Xu H, Lau SY, Liu L, et al. Nasal prevention of SARS-CoV-2 infection by intranasal influenza-based boost vaccination in mouse models. EBioMedicine. 2022;75:103762. Epub 2021 Dec 21.
49.
Food and Drug Administration. FDA approves first treatment for COVID-19. Silver Spring: FDA; 2020.
50.
Yadav DK, Singh A, Zhang Q, et al. Live attenuated avian orthoavulavirus 1-based intranasal vaccine protects hamsters from SARS-CoV-2 infection and disease. Commun Biol. 2022;5(1):316. PMID: 35338286; PMCID: PMC8957143.
51.
Rappuoli R, De Gregorio E, Del Giudice G, Phogat S, Pecetta S, Pizza M, et al. Vaccinology in the post COVID-19 era. Proc Natl Acad Sci U S A. 2021 Jan 19;118(3):e2020368118.
Udostępnij
ARTYKUŁ POWIĄZANY
Przetwarzamy dane osobowe zbierane podczas odwiedzania serwisu. Realizacja funkcji pozyskiwania informacji o użytkownikach i ich zachowaniu odbywa się poprzez dobrowolnie wprowadzone w formularzach informacje oraz zapisywanie w urządzeniach końcowych plików cookies (tzw. ciasteczka). Dane, w tym pliki cookies, wykorzystywane są w celu realizacji usług, zapewnienia wygodnego korzystania ze strony oraz w celu monitorowania ruchu zgodnie z Polityką prywatności. Dane są także zbierane i przetwarzane przez narzędzie Google Analytics (więcej).
Możesz zmienić ustawienia cookies w swojej przeglądarce. Ograniczenie stosowania plików cookies w konfiguracji przeglądarki może wpłynąć na niektóre funkcjonalności dostępne na stronie.
Możesz zmienić ustawienia cookies w swojej przeglądarce. Ograniczenie stosowania plików cookies w konfiguracji przeglądarki może wpłynąć na niektóre funkcjonalności dostępne na stronie.