RESEARCH PAPER
Quality of life of patients with implanted devices for permanent cardiac pacing assessed with the SF-36v2 Health Survey
1
Collegium Medicum, Uniwersytet Jana Kochanowskiego, Kielce, Polska
Corresponding author
Med Og Nauk Zdr. 2021;27(2):169-174
KEYWORDS
TOPICS
ABSTRACT
Objectives:
The aim of the study was comparative analysis of the quality of life of patients before and after implantation of permanent pacing devices in individual health domains of the SF-36v2 Health Survey
Material and methods:
The study group included 131 patients undergoing implantation procedures of various types of pacing systems during the period from May 2016 – March 2018 at the 2nd Department of Cardiology at the Świętokrzyskie Cardiology Center in Kielce. The study was carried out by the method of a diagnostic survey using the SF-36v2 Health Survey questionnaire. The analysis was based on a comparison of survey data collected from patients admitted to the Department of Cardiology for PM / ICD / CRT implantation and information obtained within 6–12 months after the procedure. For statistical conclusions, the level of significance was set at p=0.05.
Results:
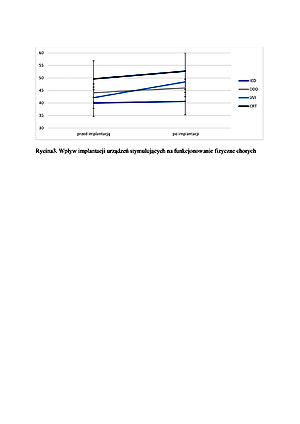
The study showed that the greatest change in quality of life after implantation according to the physical functioning subscale was observed in the case of VVI devices, and the mental health subscale in patients with CRT (p = 0.039). The vitality of all patients after implantation improved. VT: F (1; 126) = 20.99; p <0.001; ω2 = 0.14. The highest quality of life in the VT domain was observed in patients qualified for DDD pacemaker implantation, while the lowest in patients with ICD implantation (p = 0.032).
Conclusions:
Implantation of all types of permanent pacing devices contributes to the improvement of the quality of life in the following subscales of the SF-36v2 Health Survey: physical functioning (PF), role limitation in physical functioning (RP), vitality (VT) and mental health (MH). Due to the analyzes based to-date on small patient populations, further research is needed to draw conclusions concerning other benefits and problems associated with the use of devices for continuous pacing.
The aim of the study was comparative analysis of the quality of life of patients before and after implantation of permanent pacing devices in individual health domains of the SF-36v2 Health Survey
Material and methods:
The study group included 131 patients undergoing implantation procedures of various types of pacing systems during the period from May 2016 – March 2018 at the 2nd Department of Cardiology at the Świętokrzyskie Cardiology Center in Kielce. The study was carried out by the method of a diagnostic survey using the SF-36v2 Health Survey questionnaire. The analysis was based on a comparison of survey data collected from patients admitted to the Department of Cardiology for PM / ICD / CRT implantation and information obtained within 6–12 months after the procedure. For statistical conclusions, the level of significance was set at p=0.05.
Results:
The study showed that the greatest change in quality of life after implantation according to the physical functioning subscale was observed in the case of VVI devices, and the mental health subscale in patients with CRT (p = 0.039). The vitality of all patients after implantation improved. VT: F (1; 126) = 20.99; p <0.001; ω2 = 0.14. The highest quality of life in the VT domain was observed in patients qualified for DDD pacemaker implantation, while the lowest in patients with ICD implantation (p = 0.032).
Conclusions:
Implantation of all types of permanent pacing devices contributes to the improvement of the quality of life in the following subscales of the SF-36v2 Health Survey: physical functioning (PF), role limitation in physical functioning (RP), vitality (VT) and mental health (MH). Due to the analyzes based to-date on small patient populations, further research is needed to draw conclusions concerning other benefits and problems associated with the use of devices for continuous pacing.
REFERENCES (18)
1.
Steffen MM, Osborn JS, Cutler MJ. Cardiac Implantable Electronic Device Therapy: Permanent Pacemakers, Implantable Cardioverter Defibrillators, and Cardiac Resynchronization Devices. Med Clin North Am 2019; 103(5):931–943. https://doi.org/10.1016/j.mcna....
2.
Baumann K. Jakość życia w okresie późnej dorosłości – dyskurs teoretyczny. Gerontologia Polska 2006; 14(4): 165–171.
3.
Dziurowicz-Kozłowska A. Wokół pojęcia jakości życia. Psychologia Jakości Życia 2002; 1(2): 77–99.
4.
Zielińska-Więczkowska H, Kędziora-Kornatowska K. Determinanty satysfakcji życiowej w późnej dorosłości – w świetle rodzimych doniesień badawczych. Psychogeriatria Polska 2010; 7(1): 11–16.
5.
Salim S, Yamin M, Alwi I, Setiati S. Validity and Reliability of the Indonesian Version of SF-36 Quality of Life Questionnaire on Patients with Permanent Pacemakers. Acta Med Indones 2017; 49(1):10–16.
6.
Fedyk-Łukasik M. Grodzicki T. Ocena jakości życia u pacjentów z niewydolnością serca. Gerontologia Polska 2010; 18(1):16–22.
7.
Cieślik B, Podbielska H. Przegląd wybranych kwestionariuszy oceny jakości życia. Acta Bio-Optica et Informatica Medica. Inżynieria Biomedyczna 2015; 21(2): 102–135.
8.
Hindricks G, Camm J, Merkely B, Raatikainen P, Arnar DO. The EHRA White Book (online) 2017; https://www.escardio.org/stati....
9.
George D, Mallery M. SPSS for Windows Step by Step: A Simple Guide and Reference, 17.0 Update. Allyn & Bacon. Boston 2010.
10.
Udo EO, van Hemel NM, Zuithoff NP, et al. Long term quality-of-life in patients with bradycardia pacemaker implantation. Int J Cardiol 2013; 168(3): 2159–2163. https://doi.org/10.1016/j.ijca....
11.
Yardımcı T, Mert H. Web-Based Intervention to Improve Implantable Cardioverter Defibrillator Patients› Shock-Related Anxiety and Quality of Life: A Randomized Controlled Trial. Clinical Nursing Research 2019; 28(2), 150–164. https://doi.org/10.1177/105477....
12.
Cesarino CB, Beccaria LM, Aroni MM, et al. Qualidade de vida em pacientes com cardioversor desfibrilador implantável: utilização do questionário SF-36. Revista Brasileira de Cirurgia Cardiovascular 2011; 26(2): 238–243. https://doi.org/10.1590/S0102–....
13.
Hoth KF, Nash J, Poppas A, et al. Effects of cardiac resynchronization therapy on health-related quality of life in older adults with heart failure. Clinical Interventions in Aging 2008; 3(3): 553–560. https://doi.org/10.2147/cia.s1....
14.
Gomes TB, Gomes LS, de Freitas Antônio IH, et al. Avaliação da qualidade de vida pós-implante de marcapasso cardíaco artificial. Revista Eletrônica de Enfermagem 2011; 13: 735–42.
15.
Sá L, Rassi S, Batista M. Is conventional cardiac pacing harmful in patients with normal ventricular function? Arq Bras Cardiol 2013; 101(6): 545–553. http://doi.org/10.5935/abc.201....
16.
Ford J, Sears S, Ramza B, et al. The Registry Evaluating Functional Outcomes of Resynchronization Management (REFORM): quality of life and psychological functioning in patients receiving cardiac resynchronization therapy. Journal of Cardiovascular Electrophysiology 2014; 25(1): 43–51. https://doi.org/10.1111/jce.12....
17.
Knackstedt C, Arndt M, Mischke K, et al. Depression, psychological distress, and quality of life in patients with cardioverter defibrillator with or without cardiac resynchronization therapy. Heart Vessels 2014; 29(3): 364–374.
18.
Tjong FVY, Beurskens NEG, de Groot JR, et al. Health-related quality of life impact of a transcatheter pacing system. Journal of Cardiovascular Electrophysiology 2018; 29(12): 1697–1704. https://doi.org/10.1111/jce.13....
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.