RESEARCH PAPER
Urinary incontinence in patients receiving medical care in selected health service facilities in the Łódź region, Poland
1
Department of Social Medicine, Medical University, Łódź, Poland
2
Faculty of Health Sciences, Medical University, Łódź, Poland
3
Faculty of Medicine, Medical University, Łódź, Poland
Med Og Nauk Zdr. 2022;28(4):316-321
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Female physiological urinary incontinence may occur in the reproductive age, but the incidence of uncontrolled urination increases in the postmenopausal period. Urinary incontinence is playing an increasingly important social and economic role. In recent years, there has been a marked increase in the number of patients affected by incontinence symptoms presenting to the doctor due to urinary tract diseases. The main aim of the study was to investigate the prevalence of urinary incontinence among patients receiving medical care in selected institutions located in the Łódz region of Poland, and factors increasing risk of the disease.
Material and methods:
The study was conducted between January – September 2021 among women receiving health care in selected facilities in the Łódż region. The study was conducted with the use of the authors’ original, anonymous survey questionnaire consisting of 43 questions. The patients were asked to complete the survey questionnaire while waiting for an appointment at the doctor’s surgery. Completed survey questionnaires were returned by 117 women.
Results:
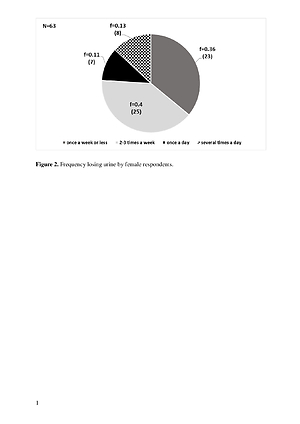
Of the 117 interviewed women, the majority, i.e. 63 people (53.9%), admitted that they had noticed the problem of incontinence. Of these 63 women, the largest number, i.e. 25 (f=0.4), admitted to losing urine 2–3 times a week.
Conclusions:
In view of the high prevalence of urinary incontinence among the studied women, there is a need to take action to disseminate knowledge about risk factors and methods of prevention of incontinence.
Female physiological urinary incontinence may occur in the reproductive age, but the incidence of uncontrolled urination increases in the postmenopausal period. Urinary incontinence is playing an increasingly important social and economic role. In recent years, there has been a marked increase in the number of patients affected by incontinence symptoms presenting to the doctor due to urinary tract diseases. The main aim of the study was to investigate the prevalence of urinary incontinence among patients receiving medical care in selected institutions located in the Łódz region of Poland, and factors increasing risk of the disease.
Material and methods:
The study was conducted between January – September 2021 among women receiving health care in selected facilities in the Łódż region. The study was conducted with the use of the authors’ original, anonymous survey questionnaire consisting of 43 questions. The patients were asked to complete the survey questionnaire while waiting for an appointment at the doctor’s surgery. Completed survey questionnaires were returned by 117 women.
Results:
Of the 117 interviewed women, the majority, i.e. 63 people (53.9%), admitted that they had noticed the problem of incontinence. Of these 63 women, the largest number, i.e. 25 (f=0.4), admitted to losing urine 2–3 times a week.
Conclusions:
In view of the high prevalence of urinary incontinence among the studied women, there is a need to take action to disseminate knowledge about risk factors and methods of prevention of incontinence.
REFERENCES (26)
1.
Barcz E. Nietrzymanie moczu u kobiet: podstawy diagnostyki i terapii. Wydawnictwo Lekarskie PZWL; 2019.
2.
Aoki Y, Brown HW, Brubaker L, et al. Urinary incontinence in women. Nat Rev Dis Primers. 2017;3:17042. https://doi.org/10.1038/nrdp.2....
3.
Hu JS, Pierre EF. Urinary incontinence in women: evaluation and management. Am Fam Physician. 2019;100(6):339–48.
4.
Blaivas JG, Olsson CA. Stress incontinence: classification and surgical approach. J Urol. 1988;139(4):727–31. https://doi.org/10.1016/s0022-....
5.
Burzyński B, Kwiatkowska K, Sołtysiak-Gibała Z, et al. Impact of stress urinary incontinence on female sexual activity. Eur Rev Med Pharmacol Sci. 2021;25(2):643–53. https://doi.org/10.26355/eurre....
6.
Zhang RQ, Xia MC, Cui F, et al. Epidemiological survey of adult female stress urinary incontinence. BMC Womens Health. 2021;21(1):172. https://doi.org/10.1186/s12905....
7.
Zincir H, Demir G, Günaydin Y, et al. Sexual Dysfunction in Married Women With Urinary Incontinence. Urol J. 2018;15(4):193–8. https://doi.org/10.22037/uj.v0....
8.
Wyndaele M, Hashim H. Pathophysiology of urinary incontinence. Surgery (Oxford). 2020;38(4):185–90.
9.
Pearlman A, Kreder K. Evaluation and treatment of urinary incontinence in the aging male. Postgrad Med. 2020;132(sup4):9–17 https://doi.org/10.1080/003254....
10.
Nazarko L. Male urinary incontinence management: penile sheaths. Br J Community Nurs. 2018;23(3):110–6. https://doi.org/10.12968/bjcn.....
11.
Hunskaar S, Burgio K, Clark A, et al. Epidemiology of urinary and faecal incontinence and pelvic organ prolapse. In: Abrams P, Cardozo L, Khoury R, et al. editors. Incontinence. 3rd international consultation on incontinence. Plymouth (United Kingdom): Health Publication Ltd; 2005. p. 255–312.
12.
Loh KY, Sivalingam N. Urinary incontinence in the elderly population. Med J Malaysia. 2006; 61(4): 506–10.
13.
Mota RL. Female urinary incontinence and sexuality. Int Braz J Urol. 2017; 43(1): 20–8. https://doi.org/10.1590/S1677-....
14.
Kołodyńska G, Zalewski M, Rożek-Piechura K. Urinary incontinence in postmenopausal women – causes, symptoms, treatment. Prz Menopauzalny. 2019;18(1):46–50. https://doi.org/10.5114/pm.201....
15.
Chu CM, Arya LA, Andy UU. Impact of urinary incontinence on female sexual health in women during midlife. Womens Midlife Health. 2015; 1: 6. https://doi.org/10.1186/s40695....
16.
Denisenko AA, Clark CB, D’Amico M, et al. Evaluation and management of female urinary incontinence. Can J Urol. 2021;28(S2):27–32.
17.
Mallah F, Montazeri A, Ghanbari Z, et al. Effect of urinary incontinence on quality of life among iranian women. J Family Reprod Health. 2014; 8(1):13–9.
18.
Goforth J, Langaker M. Urinary Incontinence in Women. N C Med J. 2016;77(6):423–5. https://doi.org/10.18043/ncm.7....
19.
Wyndaele JJ, Kovindha A, Madersbacher H, et al. Neurologic urinary incontinence. Neurourol Urodyn. 2010;29(1):159164. https://doi.org/10.1002/nau.20....
20.
Prażmowska B, Puto G, Gergont B. Wpływ nietrzymania moczu na satysfakcję z życia kobiet po 45 roku życia. Probl Hig Epidemiol. 2012:93(4): 785–9.
21.
Stadnicka G, Janik M, Łepecka-Klusek C, et al. Psychospołeczne następstwa nietrzymania moczu. Med Og Nauk Zdr. 2014;20(2):136-140.
22.
Klimaszewska K, Bartusek M. Urinary incontinence as the socioeconomic problem. Pielęgniarstwo XXI wieku /Nursing in the 21st Century. 2017;16(3):62–6. https://doi.org/10.1515/pielxx....
23.
Saboia DM, Firmiano MLV, Bezerra KC, et al. Impact of urinary incontinence types on women's quality of life. Rev Esc Enferm USP. 2017;51:e03266. https://doi.org/10.1590/S1980-....
24.
Nygaard CC, Schreiner L, Morsch TP, et al. Urinary incontinence and quality of life in female patients with obesity. Rev Bras Ginecol Obstet. 2018;40(9):534–9. https://doi.org/10.1055/s-0038....
25.
Almutairi S, Alobaid O, Al-Zahrani MA, et al. Urinary incontinence among Saudi women: prevalence, risk factors, and impact on quality of life. Eur Rev Med Pharmacol Sci. 2021;25(20):6311–8. https://doi. org/10.26355/eurrev_202110_27001.
26.
Pizzol D, Demurtas J, Celotto S, et al. Urinary incontinence and quality of life: a systematic review and meta-analysis. Aging Clin Exp Res. 2021; 33(1):25–35. https://doi.org/10.1007/s40520....
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.