REVIEW PAPER
Is the condition of the digestive tract, alcohol and supplements available for soluble absorption?
1
Department and Clinic of Gastroenterology, Dietetics and Internal Medicine, K. Marcinkowski University of Medical Sciences in Poznań, Poland., Poznań University of Medical Sciences: Poznań, PL, Polska
These authors had equal contribution to this work
Corresponding author
Klara Szwarc
Katedra i Klinika Gastroenterologii, Dietetyki i Chorób Wewnętrznych Uniwersytetu Medycznego im K. Marcinkowskiego w Poznaniu, Polska
Katedra i Klinika Gastroenterologii, Dietetyki i Chorób Wewnętrznych Uniwersytetu Medycznego im K. Marcinkowskiego w Poznaniu, Polska
Med Og Nauk Zdr. 2025;31(4):219-224
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Drug-food interactions are an increasingly common problem, especially in developed countries. Elderly people are particularly susceptible to this phenomenon, as they often struggle with intestinal dysbiosis, digestive and motility disorders, and other conditions, which translates into the need to use large amounts of pharmaceuticals and dietary supplements. The aim of the study is to review the current knowledge on the impact of gastrointestinal conditions and the consumption of alcohol and dietary supplements on drug interactions.
Review methods:
The study was conducted based on research found in the Google Scholar browser and the PubMed database using the key words ‘alcohol, microbiota’, ‘dietary supplements’, and ‘drugs’.
Brief description of the state of knowledge:
Most known drug-food interactions occur during absorption. The presence of food and fluid in the gastrointestinal tract can modify both the composition of the gut microbiota and the state of the intestinal barrier, which can impact the effectiveness of therapy. However, consuming alcohol or dietary supplements shortly after taking medications can either increase or decrease the effectiveness of individual medications.
Summary:
Therefore, it is important to educate both medical staff and patients about possible interactions between individual food ingredients and medications, as well as the importance of maintaining a healthy gut microbiota, which will optimize treatment and minimize the risk of side effects.
Drug-food interactions are an increasingly common problem, especially in developed countries. Elderly people are particularly susceptible to this phenomenon, as they often struggle with intestinal dysbiosis, digestive and motility disorders, and other conditions, which translates into the need to use large amounts of pharmaceuticals and dietary supplements. The aim of the study is to review the current knowledge on the impact of gastrointestinal conditions and the consumption of alcohol and dietary supplements on drug interactions.
Review methods:
The study was conducted based on research found in the Google Scholar browser and the PubMed database using the key words ‘alcohol, microbiota’, ‘dietary supplements’, and ‘drugs’.
Brief description of the state of knowledge:
Most known drug-food interactions occur during absorption. The presence of food and fluid in the gastrointestinal tract can modify both the composition of the gut microbiota and the state of the intestinal barrier, which can impact the effectiveness of therapy. However, consuming alcohol or dietary supplements shortly after taking medications can either increase or decrease the effectiveness of individual medications.
Summary:
Therefore, it is important to educate both medical staff and patients about possible interactions between individual food ingredients and medications, as well as the importance of maintaining a healthy gut microbiota, which will optimize treatment and minimize the risk of side effects.
REFERENCES (46)
1.
Wierzba K, Chmielewski M, Błeszyńska-Marunowska E, et al. Regular Use of Oral Nonsteroidal Anti-inflammatory Drugs in a Population of Polish Seniors: Findings from the PolSenior2 Cross-Sectional Survey. Drugs Aging. 2025;42(3):245–55. https://doi.org/10.1007/s40266....
2.
Sobotta Ł, Suliburska JM, Mielcarek J. Interakcje leków z żywnością. Bromat Chem Toksykol. -XLIV. 2011;1: 95–103.
3.
Koziolek M, Alcaro S, Augustijns P, et al. The mechanisms of pharmacokinetic food-drug interactions – A perspective from the UNGAP group. European Journal of Pharmaceutical Sciences. 2019;134:31–59.https://doi.org/10.1016/j.ejps....
4.
Deng J, Zhu X, Chen Z, et al. A Review of Food-Drug Interactions on Oral Drug Absorption. Drugs. 2017;77(17):1833–55.https://doi.org/10.1007/s40265....
5.
Berg G, Rybakova D, Fischer D, et al. Microbiome definition re-visited: old concepts and new challenges. Microbiome. 2020;30;8(1):103. https://doi.org/10.1186/s40168....
6.
Becker HEF, Demers K, Derijks LJJ, et al. Current evidence and clinical relevance of drug-microbiota interactions in inflammatory bowel disease. Front Microbiol. 2023;14:1107976. https://doi.org/10.3389/fmicb.....
7.
Suliburska J. Ocena interakcji leków hipotensyjnych ze składnikami żywności i suplementami diety u pacjentów z nadciśnieniem tętniczym. Bromat.chem.toksykol-XLIII. 2010;1:35–40.
8.
Hua R, Lam CS, Wu YK, et al. The use of potentially interacting supplement-drug pairs in adults with type 2 diabetes: A large population-based cohort study in the UK Biobank. Diabetes Res Clin Pract. 2024;211:111658. https://doi.org/10.1016/j.diab....
9.
Cummings JH, Antoine JM, Azpiroz F, et al. PASSCLAIM--gut health and immunity. Eur J Nutr. 2004;43 Suppl 2: II118–73. https://doi.org/10.1007/s00394....
10.
Chen K, Wang H, Yang Y, et al. Common mechanisms of Gut microbe-based strategies for the treatment of intestine-related diseases: based on multi-target interactions with the intestinal barrier. Cell Communication and Signaling. 2025;18;23(1):288. https://doi.org/10.1186/s12964....
11.
Vancamelbeke M, Vermeire S. The intestinal barrier: a fundamental role in health and disease. Expert Rev Gastroenterol Hepatol. 2017;11(9):821–34. https://doi.org/10.1080/174741....
12.
Leibovitzh H, Lee SH, Xue M, et al. Altered Gut Microbiome Composition and Function Are Associated With Gut Barrier Dysfunction in Healthy Relatives of Patients With Crohn’s Disease. Gastroenterology. 2022;163(5):1364–1376.e10. https://doi.org/10.1053/j.gast....
13.
Dunleavy KA, Raffals LE, Camilleri M. Intestinal Barrier Dysfunction in Inflammatory Bowel Disease: Underpinning Pathogenesis and Therapeutics. Dig Dis Sci. 2023;68(12):4306–20. https://doi.org/10.1007/s10620....
14.
Cukrowska B, Sowińska A, Bierła JB, et al. Intestinal epithelium, intraepithelial lymphocytes and the gut microbiota – Key players in the pathogenesis of celiac disease. World J Gastroenterol. 2017;14;23(42):7505–18. https://doi.org/10.3748/wjg.v2....
15.
Pisani A, Rausch P, Bang C, et al. Dysbiosis in the Gut Microbiota in Patients with Inflammatory Bowel Disease during Remission. Microbiol Spectr. 2022;29;10(3):e0061622. https://doi.org/10.1128/spectr....
16.
Kushkevych I, Dvořáková M, Dordevic D, et al. Advances in gut microbiota functions in inflammatory bowel disease: Dysbiosis, management, cytotoxicity assessment, and therapeutic perspectives. Comput Struct Biotechnol J. 2025;27:851–68. https://doi.org/10.1016/j.csbj....
17.
Hanning N, Edwinson AL, Ceuleers H, et al. Intestinal barrier dysfunction in irritable bowel syndrome: a systematic review. Therap Adv Gastroenterol. 2021;14:1756284821993586. https://doi.org/10.1177/175628....
18.
Odenwald MA, Turner JR. The intestinal epithelial barrier: a therapeutic target? Nat Rev Gastroenterol Hepatol. 2017;14(1):9–21. https://doi.org/10.1038/nrgast....
19.
Rath T, Atreya R, Neurath MF. A spotlight on intestinal permeability and inflammatory bowel diseases. Expert Rev Gastroenterol Hepatol. 2023;17(9):893–902. https://doi.org/10.1080/174741....
20.
Turpin W, Lee SH, Raygoza Garay JA, et al. Increased Intestinal Permeability Is Associated With Later Development of Crohn’s Disease. Gastroenterology. 2020;159(6):2092–2100.e5. https://doi.org/10.1053/j.gast....
21.
Fine-Shamir N, Dahan A. Solubility-enabling formulations for oral delivery of lipophilic drugs: considering the solubility-permeability interplay for accelerated formulation development. Expert Opin Drug Deliv. 2024;21(1):13–29. https://doi.org/10.1080/174252....
22.
Markovic M, Zur M, Ragatsky I, et al. BCS Class IV Oral Drugs and Absorption Windows: Regional-Dependent Intestinal Permeability of Furosemide. Pharmaceutics. 2020;2;12(12):1175. https://doi.org/10.3390/pharma....
23.
Singh RS, Singh A, Batra G, et al. Novel targets for drug discovery in celiac disease. Indian J Pharmacol. 2019;51(5):359–65. https://doi.org/10.4103/ijp.ij....
24.
Hatton GB, Madla CM, Rabbie SC, et al. Gut reaction: impact of systemic diseases on gastrointestinal physiology and drug absorption. Drug Discov Today. 2019;24(2):417–27. https://doi.org/10.1016/j.drud....
25.
Vinarov Z, Abdallah M, Agundez JAG, et al. Impact of gastrointestinal tract variability on oral drug absorption and pharmacokinetics: An UNGAP review. Eur J Pharm Sci. 2021;162:105812. https://doi.org/10.1016/j.ejps....
26.
Nakai D, Miyake M. Intestinal Membrane Function in Inflammatory Bowel Disease. Pharmaceutics. 2023;25;16(1):29. https://doi.org/10.3390/pharma....
27.
Crouwel F, Buiter HJC, de Boer NK. Gut microbiota-driven drug metabolism in inflammatory bowel disease. J Crohns Colitis. 2020;11;15(2):307–15. https://doi.org/10.1093/ecco-j....
28.
Sousa T, Yadav V, Zann V, et al. On the colonic bacterial metabolism of azo-bonded prodrugsof 5-aminosalicylic acid. J Pharm Sci. 2014;103(10):3171–5. https://doi.org/10.1002/jps.24....
29.
Radhakrishnan ST, Alexander JL, Mullish BH, et al. Systematic review: the association between the gut microbiota and medical therapies in inflammatory bowel disease. Aliment Pharmacol Ther. 2022;55(1):26–48. https://doi.org/10.1111/apt.16....
30.
Alexandrescu L, Nicoara AD, Tofolean DE, et al. Healing from Within: How Gut Microbiota Predicts IBD Treatment Success-A Systematic Review. Int J Mol Sci. 2024;2;25(15):8451. https://doi.org/10.3390/ijms25....
31.
Mah C, Jayawardana T, Leong G, et al. Assessing the Relationship between the Gut Microbiota and Inflammatory Bowel Disease Therapeutics: A Systematic Review. Pathogens. 2023;6;12(2):262. https://doi.org/10.3390/pathog....
32.
Wada H, Miyoshi J, Kuronuma S, et al. 5-Aminosalicylic acid alters the gut microbiota and altered microbiota transmitted vertically to offspring have protective effects against colitis. Sci Rep. 2023;28;13(1):12241. https://doi.org/10.1038/s41598....
33.
Zhao Q, Chen Y, Huang W, et al. Drug-microbiota interactions: an emerging priority for precision medicine. Signal Transduct Target Ther. 2023;9;8(1):386. https://doi.org/10.1038/s41392....
34.
Fagerberg JH, Sjögren E, Bergström CAS. Concomitant intake of alcohol may increase the absorption of poorly soluble drugs. Eur J Pharm Sci. 2015;25;67:12–20. https://doi.org/10.1016/j.ejps....
35.
Jung YH, Heo DG, Lee DC, et al. Effect of concomitant oral administration of ethanol on the pharmacokinetics of nicardipine in rats. Biomed Chromatogr. 2022;36(9):e5425. https://doi.org/10.1002/bmc.54....
36.
Zhu Q, Xie X, Fang L, et al. Chronic alcohol intake disrupts cytochrome P450 enzyme activity in alcoholic fatty liver disease: insights into metabolic alterations and therapeutic targets. Front Chem. 2025;13;13:1509785.
37.
Mergenhagen KA, Wattengel BA, Skelly MK, et al. Fact versus Fiction: a Review of the Evidence behind Alcohol and Antibiotic Interactions. Antimicrob Agents Chemother. 2020 21;64(3):e02167–19. https://doi.org/10.1128/aac.02....
38.
Weathermon R, Crabb DW. Alcohol and medication interactions. Alcohol Res Health. 1999;23(1):40–54.
39.
Ridout F, Shamsi Z, Meadows R, et al. A single-center, randomized, double-blind, placebo-controlled, crossover investigation of the effects of fexofenadine hydrochloride 180 mg alone and with alcohol, with hydroxyzine hydrochloride 50 mg as a positive internal control, on aspects of cognitive and psychomotor function related to driving a car. Clin Ther. 2003;25(5):1518–38. https://doi.org/10.1016/s0149-....
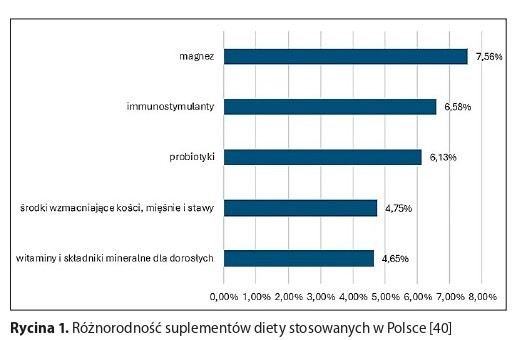
40.
Goryńska-Goldmann, Kobusowska E, Dziedziński J, et al. Problem nadmiernego spożycia suplementów diety wśród ludności polskiej. 2019;235–242.
41.
Suliburska J, Bogdański P. Ocena sposobu żywienia, stanu odżywienia i ryzyka interakcji pokarmowo-lekowych u pacjentów z cukrzycą typu 2. Farmacja Współczesna. 2011;4:3–8.
42.
Cheng W, Xia K, Wu S, et al. Herb-Drug Interactions and Their Impact on Pharmacokinetics: An Update. Curr Drug Metab. 2023;24(1):28–69. https://doi.org/10.2174/138920....
43.
Mieszkowska M, Michota-Katulska E. Suplementy diety – korzyści i skutki uboczne. Bezpieczeństwo pracy: nauka i praktyka. 2008;(6):28–30.
44.
Johnson MA. Influence of vitamin K on anticoagulant therapy depends on vitamin K status and the source and chemical forms of vitamin K. Nutr Rev. 2005;63(3):91–7. https://doi.org/10.1111/j.1753....
45.
Jun JE, Jeong IK, Yu JM, et al. Efficacy and Safety of Omega-3 Fatty Acids in Patients Treated with Statins for Residual Hypertriglyceridemia: A Randomized, Double-Blind, Placebo-Controlled Clinical Trial. Diabetes Metab J. 2020 Feb;44(1):78–90. https://doi.org/10.4093/dmj.20....
46.
Okello E, Jiang X, Mohamed S, et al. Combined statin/coenzyme Q10 as adjunctive treatment of chronic heart failure. Med Hypotheses. 2009 Sep;73(3):306–8. https://doi.org/10.1016/j.mehy....
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.