REVIEW PAPER
Effect of electronic nicotine delivery systems on upper respiratory tract microbiota and pathogenesis of selected respiratory diseases
1
Students Scientific Association at
the Chair and Department of Medical
Microbiology, Medical University of Lublin, Polska
2
Chair and Department of Medical Microbiology, Medical University of Lublin (Poland), Polska
These authors had equal contribution to this work
Corresponding author
Małgorzata Maria Kozioł
Katedra i Zakład Mikrobiologii Lekarskiej, Uniwersytet Medyczny w Lublinie, ul. Chodźki 1, 20-059, Lublin, Polska
Katedra i Zakład Mikrobiologii Lekarskiej, Uniwersytet Medyczny w Lublinie, ul. Chodźki 1, 20-059, Lublin, Polska
Med Og Nauk Zdr. 2025;31(4):245-252
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
In recent years, electronic nicotine delivery systems (ENDS) have gained popularity as an alternative to traditional cigarettes. While the impact of conventional smoking on the oral microbiota is well documented, the influence of e-cigarettes on upper respiratory tract (URT) microbiota and diseases, such as asthma or chronic obstructive pulmonary disease (COPD), remains poorly understood. The aim of this study is to analyze available research on the effects of ENDS on the composition and function of the URT microbiota.
Review methods:
A literature review was conducted using the PubMed database, with publications selected based on relevant keywords. Additionally, the study was supplemented with statistical data from Polish and international sources (Gov, WHO, FDA).
Brief description of the state of knowledge:
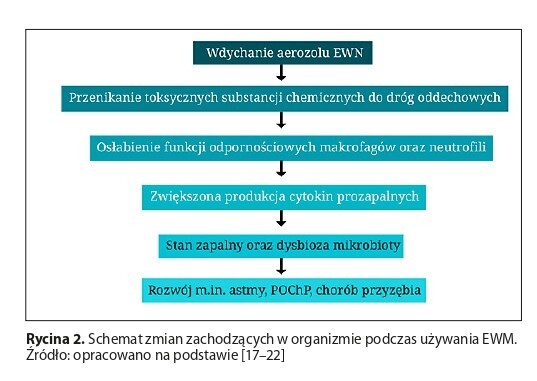
In Poland, the number of e-cigarette units sold in 2023 reached 100 million. The ENDS aerosol can significantly disrupt the microbial balance, increasing the number of pathogenic microorganisms. Various chemical substances, such as nicotine, heavy metals, and aldehydes, may damage mucosal membranes, induce oxidative stress, and increase the production of pro-inflammatory cytokines, ultimately contributing to the development of numerous respiratory pathologies. Exposure to the aerosol significantly contributes to the exacerbation of asthma attacks and increases the risk of developing chronic obstructive pulmonary disease (COPD).
Summary:
Current research indicates that regular use of END -both active and passive—can lead to dysbiosis of URT, increasing the risk of developing respiratory diseases. Unfortunately, the diversity of ENDS types and the complexity of their design hinder the interpretation of research findings. Moreover, there is a lack of significant data regarding the longterm health effects of electronic nicotine delivery systems.
In recent years, electronic nicotine delivery systems (ENDS) have gained popularity as an alternative to traditional cigarettes. While the impact of conventional smoking on the oral microbiota is well documented, the influence of e-cigarettes on upper respiratory tract (URT) microbiota and diseases, such as asthma or chronic obstructive pulmonary disease (COPD), remains poorly understood. The aim of this study is to analyze available research on the effects of ENDS on the composition and function of the URT microbiota.
Review methods:
A literature review was conducted using the PubMed database, with publications selected based on relevant keywords. Additionally, the study was supplemented with statistical data from Polish and international sources (Gov, WHO, FDA).
Brief description of the state of knowledge:
In Poland, the number of e-cigarette units sold in 2023 reached 100 million. The ENDS aerosol can significantly disrupt the microbial balance, increasing the number of pathogenic microorganisms. Various chemical substances, such as nicotine, heavy metals, and aldehydes, may damage mucosal membranes, induce oxidative stress, and increase the production of pro-inflammatory cytokines, ultimately contributing to the development of numerous respiratory pathologies. Exposure to the aerosol significantly contributes to the exacerbation of asthma attacks and increases the risk of developing chronic obstructive pulmonary disease (COPD).
Summary:
Current research indicates that regular use of END -both active and passive—can lead to dysbiosis of URT, increasing the risk of developing respiratory diseases. Unfortunately, the diversity of ENDS types and the complexity of their design hinder the interpretation of research findings. Moreover, there is a lack of significant data regarding the longterm health effects of electronic nicotine delivery systems.
REFERENCES (53)
1.
Kramarow EA, Elgaddal N. Current Electronic Cigarette Use Among Adults Aged 18 and Over: United States, 2021. NCHS Data Brief. 2023;(475):1–8. https://www.cdc.gov/nchs/data/... (access: 2025.06.28).
2.
Chattopadhyay S, Malayil L, Chopyk J, et al. Oral microbiome dysbiosis among cigarette smokers and smokeless tobacco users compared to non-users. Sci Rep. 2024;14(1):10394. doi:10.1038/s41598-024-60730-2.
3.
Ceasar RC, Braymiller JL, Kechter A, et al. Perceiving E-Cigarettes as Safe and Safer Alternative to Cigarettes Among Young Adults. Subst Use Addctn J. 2024;45(2):181–190. doi:10.1177/29767342231218533.
4.
World Health Organization Tobacco. Key Facts. Available online: https://www.who.int/news-room/... (access: 2025.06.28).
5.
Powiatowa Stacja Sanitarno-epidemiologiczna. E-papierosy; gov.pl https://www.gov.pl/web/psse-py... E-papierosy – (access 2025.06.28).
6.
Jankowski M, Ostrowska A, Sierpiński R, et al. The Prevalence of Tobacco, Heated Tobacco, and E-Cigarette Use in Poland: A 2022 Web-Based Cross-Sectional Survey. Int J Environ Res Public Health. 2022;19(8):4904. doi:10.3390/ijerph19084904.
7.
Frie JA, Nolan CJ, Murray JE, Khokhar JY. Addiction-Related Outcomes of Nicotine and Alcohol Co-use: New Insights Following the Rise in Vaping. Nicotine Tob Res. 2022;24(8):1141–1149. doi:10.1093/ntr/ntab231.
8.
Ministerstwo Zdrowia. E-papierosy – rosnący problem zdrowia publicznego [Internet]. gov.pl; 2023 Available from: https://www.gov.pl/web/zdrowie... (access: 2025.06.28).
9.
Peng X, Cheng L, You Y, et al. Oral microbiota in human systematic diseases. Int J Oral Sci. 2022;14(1):14. doi:10.1038/s41368-022-00163-7.
10.
Chun LF, Moazed F, Calfee CS, Matthay MA, Gotts JE. Pulmonary toxicity of e-cigarettes. Am J Physiol Lung Cell Mol Physiol. 2017;313(2):L193-L206. doi:10.1152/ajplung.00071.2017.
11.
Audrain-McGovern J, Strasser AA, Wileyto EP. The impact of flavoring on the rewarding and reinforcing value of e-cigarettes with nicotine among young adult smokers. Drug Alcohol Depend. 2016;166:263–267. doi:10.1016/j.drugalcdep.2016.06.030.
12.
U.S. Food and Drug Administration (FDA). FDA authorizes marketing of IQOS Tobacco Heating System with “reduced exposure” information [Internet]. Silver Spring (MD): FDA; 2020 Jul 7 https://www.fda.gov/news-event... (access: 2025.04.22].
13.
Eltorai AE, Choi AR, Eltorai AS. Impact of Electronic Cigarettes on Various Organ Systems. Respir Care. 2019;64(3):328–336. doi:10.4187/respcare.06300.
14.
Eshraghian EA, Al-Delaimy WK. A review of constituents identified in e-cigarette liquids and aerosols. Tob Prev Cessat. 2021;7:10. doi:10.18332/tpc/131111.
15.
Goniewicz ML, Knysak J, Gawron M, et al. Levels of selected carcinogens and toxicants in vapour from electronic cigarettes. Tob Control. 2014;23(2):133–139. doi:10.1136/tobaccocontrol-2012-050859.
16.
Chun LF, Moazed F, Calfee CS, Matthay MA, Gotts JE. Pulmonary toxicity of e-cigarettes. Am J Physiol Lung Cell Mol Physiol. 2017;313(2):L193–L206. doi:10.1152/ajplung.00071.2017.
17.
Benowitz NL, Fraiman JB. Cardiovascular effects of electronic cigarettes. Nat Rev Cardiol. 2017;4(8):447–456. doi:10.1038/nrcardio.2017.36.
18.
Chadi N, Belanger RE. Teen vaping: There is no vapour without fire. Paediatr Child Health. 2019;25(6):337–339. doi:10.1093/pch/pxz137.
19.
Scott A, Lugg ST, Aldridge K, et al. Pro-inflammatory effects of e-cigarette vapour condensate on human alveolar macrophages. Thorax. 2018;73(12):1161–1169. doi:10.1136/thoraxjnl-2018-211663.
20.
Ghosh A, Coakley RD, Ghio AJ, et al. Chronic E-Cigarette Use Increases Neutrophil Elastase and Matrix Metalloprotease Levels in the Lung. Am J Respir Crit Care Med. 2019;200(11):1392–1401. doi:10.1164/rccm.201903-0615OC.
21.
Anderson C, Majeste A, Hanus J, Wang S. E-Cigarette Aerosol Exposure Induces Reactive Oxygen Species, DNA Damage, and Cell Death in Vascular Endothelial Cells. Toxicol Sci. 2016;154(2):332–340. doi:10.1093/toxsci/kfw166.
22.
Rouabhia M, Semlali A. Electronic cigarette vapor increases Streptococcus mutans growth, adhesion, biofilm formation, and expression of the biofilm-associated genes. Oral Dis. 2021;27(3):639–647. doi:10.1111/odi.13564.
23.
Campbell CD, Barnett C, Sulaiman I. A clinicians' review of the respiratory microbiome. Breathe (Sheff). 2022;18(1):210161. doi:10.1183/20734735.0161-2021.
24.
Schenck LP, Surette MG, Bowdish DM. Composition and immunological significance of the upper respiratory tract microbiota. FEBS Lett. 2016;590(21):3705–3720. doi:10.1002/1873-3468.12455.
25.
Charlson ES, Bittinger K, Haas AR, et al. Topographical continuity of bacterial populations in the healthy human respiratory tract. Am J Respir Crit Care Med. 2011;184(8):957–963. doi:10.1164/rccm.201104-0655OC.
26.
Prasetyo A, Sadhana U, Budiman J. Nasal Mucociliary Clearance in Smokers: A Systematic Review. Int Arch Otorhinolaryngol. 2021;25(1):e160-e169. doi:10.1055/s-0040-1702965.
27.
Pushalkar S, Paul B, Li Q, et al. Electronic Cigarette Aerosol Modulates the Oral Microbiome and Increases Risk of Infection. iScience. 2020;23(3):100884. doi:10.1016/j.isci.2020.100884.
28.
Holliday R, Chaffee BW, Jakubovics NS, Kist R, Preshaw PM. Electronic Cigarettes and Oral Health. J Dent Res. 2021;100(9):906–913. doi:10.1177/00220345211002116.
29.
Hickman E, Roca C, Zorn BT, et al. E-Cigarette Use, Cigarette Smoking, and Sex Are Associated With Nasal Microbiome Dysbiosis. Nicotine Tob Res. 2024;27(1):114–124. doi:10.1093/ntr/ntae176.
30.
Hwang JH, Lyes M, Sladewski K, et al. Electronic cigarette inhalation alters innate immunity and airway cytokines while increasing the virulence of colonizing bacteria. J Mol Med (Berl). 2016;94(6):667–679. doi:10.1007/s00109-016-1378-3.
31.
Laux C, Peschel A, Krismer B. Staphylococcus aureus Colonization of the Human Nose and Interaction with Other Microbiome Members. Microbiol Spectr. 2019;7(2):10.1128/microbiolspec.gpp3-0029-2018. doi:10.1128/microbiolspec.GPP3-0029-2018.
32.
Bagale K, Paudel S, Cagle H, Sigel E, Kulkarni R. Electronic Cigarette (E-Cigarette) Vapor Exposure Alters the Streptococcus pneumoniae Transcriptome in a Nicotine-Dependent Manner without Affecting Pneumococcal Virulence. Appl Environ Microbiol. 2020;86(3):e02125–19. doi:10.1128/AEM.02125-19.
33.
Miyashita L, Suri R, Dearing E, et al. E-cigarette vapour enhances pneumococcal adherence to airway epithelial cells. Eur Respir J. 2018;51(2):1701592. doi:10.1183/13993003.01592-2017.
34.
Pacjent.gov.pl. Czy masz astmę?; Ministerstwo Zdrowia, https://pacjent. gov.pl/jak-zyc-z-choroba/czy-masz-astme (access: 2025.06.28).
35.
World Health Organization (WHO). Asthma. Geneva: WHO; 2023. https://www.who.int/news-room/... (access: 2025.06.28).
36.
Lizzo JM, Goldin J, Cortes S. Pediatric Asthma. [Updated 2024 May 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. https://www.ncbi.nlm.nih.gov/b... (access: 2025.06.28).
37.
Zhou Y, Jackson D, Bacharier LB, et al. The upper-airway microbiota and loss of asthma control among asthmatic children. Nat Commun. 2019;10(1):5714. doi:10.1038/s41467-019-13698-x.
38.
McCauley K, Durack J, Valladares R, et al. Distinct nasal airway bacterial microbiotas differentially relate to exacerbation in pediatric patients with asthma. J Allergy Clin Immunol. 2019;144(5):1187–1197. doi:10.1016/j.jaci.2019.05.035.
39.
Durack J, Huang YJ, Nariya S, et al. Bacterial biogeography of adult airways in atopic asthma. Microbiome. 2018;6(1):104. doi:10.1186/s40168-018-0487-3.
40.
Alnajem A, Redha A, Alroumi D, et al. Use of electronic cigarettes and secondhand exposure to their aerosols are associated with asthma symptoms among adolescents: a cross-sectional study. Respir Res. 2020;21(1):300. doi:10.1186/s12931-020-01569-9.
41.
Bayly JE, Bernat D, Porter L, Choi K. Secondhand Exposure to Aerosols From Electronic Nicotine Delivery Systems and Asthma Exacerbations Among Youth With Asthma. Chest. 2019;155(1):88–93. doi:10.1016/j. chest.2018.10.005.
42.
World Health Organization (WHO). Chronic obstructive pulmonary disease (COPD); Geneva: WHO; https://www.who.int/news-room/...) (access 2025.04.22).
43.
Państwowa Stacja Sanitarno-Epidemiologiczna w Świdwinie. Światowy Dzień Przewlekłej Obturacyjnej Choroby Płuc; gov.pl 2023. https://www.gov.pl/web/psse-sw... (access: 2025.06.28).
44.
Medycyna Praktyczna. Przewlekła obturacyjna choroba płuc (POChP). Kraków: Medycyna Praktyczna; https://www.mp.pl/interna/chap... (access 2025.04.22).
45.
Polosa R, Morjaria JB, Prosperini U, et al. Health effects in COPD smokers who switch to electronic cigarettes: a retrospective prospective 3-year follow-up. Int J Chron Obstruct Pulmon Dis. 2018;13:2533–2542. doi:10.2147/COPD.S161138.
46.
Antwi GO, Rhodes DL. Association between E-cigarette use and chronic obstructive pulmonary disease in non-asthmatic adults in the USA. J Public Health (Oxf). 2022;44(1):158–164. doi:10.1093/pubmed/fdaa229.
47.
Saha P, Jain S, Mukherjee I, et al. The effects of dual IQOS and cigarette smoke exposure on airway epithelial cells: implications for lung health and respiratory disease pathogenesis. ERJ Open Res. 2023;9(3):00558–2022. doi:10.1183/23120541.00558-2022.
48.
Bozier J, Rutting S, Xenaki D, Peters M, Adcock I, Oliver BG. Heightened response to e-cigarettes in COPD. ERJ Open Res. 2019;5(1):00192–2018. doi:10.1183/23120541.00192-2018.
49.
Marin A, Garcia-Aymerich J, Sauleda J, et al. Effect of bronchial colonisation on airway and systemic inflammation in stable COPD. COPD. 2012;9(2):121–130. doi:10.3109/15412555.2011.636407.
50.
Jacobs DM, Ochs-Balcom HM, Zhao J, Murphy TF, Sethi S. Lower Airway Bacterial Colonization Patterns and Species-Specific Interactions in Chronic Obstructive Pulmonary Disease. J Clin Microbiol. 2018;56(10):e00330–18. doi:10.1128/JCM.00330-18.
51.
Rosell A, Monsó E, Soler N, et al. Microbiologic determinants of exacerbation in chronic obstructive pulmonary disease. Arch Intern Med. 2005;165(8):891–897. doi:10.1001/archinte.165.8.891.
52.
Cabrera-Rubio R, Garcia-Núñez M, Setó L, et al. Microbiome diversity in the bronchial tracts of patients with chronic obstructive pulmonary disease. J Clin Microbiol. 2012;50(11):3562–3568. doi:10.1128/ JCM.00767-12.
53.
Marin A, Monsó E, Garcia-Nuñez M, et al. Variability and effects of bronchial colonisation in patients with moderate COPD. Eur Respir J. 2010;35(2):295–302. doi:10.1183/09031936.00126808.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.