RESEARCH PAPER
Health-promoting and anti-health behaviours of workers exposed to solar radiation
1
Department of Nutrition and Epidemiology, Medical University of Łódź, Polska
2
Department of Nutrition and Epidemiology, Medical University of Łódź
3
Profamilia Medical Center
Corresponding author
Anna Garus-Pakowska
Zakład Żywienia i Epidemiologii, Uniwersytet Medyczny w Łodzi, ul Żeligowskiego 7/9, Łódź, Polska
Zakład Żywienia i Epidemiologii, Uniwersytet Medyczny w Łodzi, ul Żeligowskiego 7/9, Łódź, Polska
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Occupational exposure to solar radiation is a risk factor for skin diseases. Personal protective equipment and individual behaviours of those occupationally exposed to UV radiation are important preventative measures. The aim of this study was to assess health-related behaviours of workers exposed to solar radiation.
Material and methods:
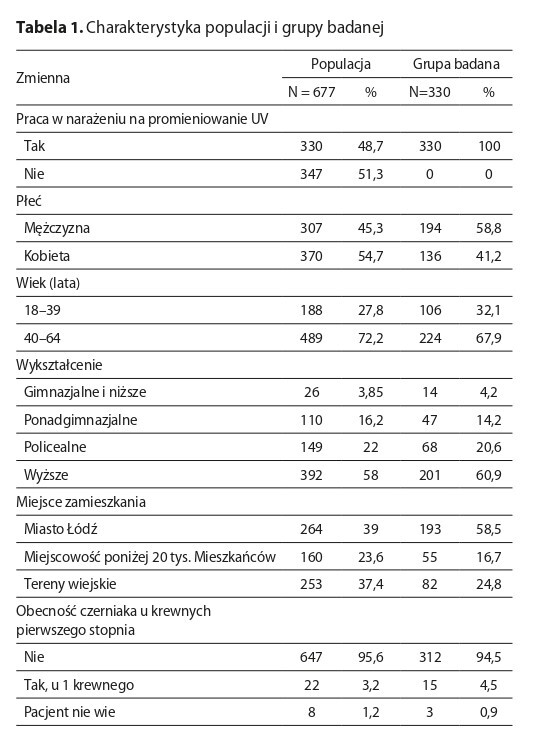
The study included 330 individuals exposed to solar radiation at work. A questionnaire was used to collect data on health-promoting and anti-health behaviours. Individuals with suspicious skin lesions were referred for dermatological examinations. Pearson‘s chi-square test or Fisher‘s exact test were used for selected variables, and the p values p < 0.05 were considered significant.
Results:
Females more often than males used sunscreen and sunglasses with UV protection (p<0.05). Despite occupational exposure, 125 people admitted they did not limit their sun exposure. The majority of respondents did not know the number of moles on their bodies, had never performed a skin self-examination, and had never had their moles checked by a dermatologist. One in four respondent had a suspicious lesion detected that required further consultation with a doctor, and 10 participants had a lesion that was cancerous.
Conclusions:
The study found that most respondents did not demonstrate sufficient health-promoting behaviours and emphasized the importance of access to screening tests. Education about the risks associated with UV exposure and participation in screening tests are of key importance and may result in the reduction of skin cancer rates, increase detection rates, and improve treatment outcomes.
Occupational exposure to solar radiation is a risk factor for skin diseases. Personal protective equipment and individual behaviours of those occupationally exposed to UV radiation are important preventative measures. The aim of this study was to assess health-related behaviours of workers exposed to solar radiation.
Material and methods:
The study included 330 individuals exposed to solar radiation at work. A questionnaire was used to collect data on health-promoting and anti-health behaviours. Individuals with suspicious skin lesions were referred for dermatological examinations. Pearson‘s chi-square test or Fisher‘s exact test were used for selected variables, and the p values p < 0.05 were considered significant.
Results:
Females more often than males used sunscreen and sunglasses with UV protection (p<0.05). Despite occupational exposure, 125 people admitted they did not limit their sun exposure. The majority of respondents did not know the number of moles on their bodies, had never performed a skin self-examination, and had never had their moles checked by a dermatologist. One in four respondent had a suspicious lesion detected that required further consultation with a doctor, and 10 participants had a lesion that was cancerous.
Conclusions:
The study found that most respondents did not demonstrate sufficient health-promoting behaviours and emphasized the importance of access to screening tests. Education about the risks associated with UV exposure and participation in screening tests are of key importance and may result in the reduction of skin cancer rates, increase detection rates, and improve treatment outcomes.
REFERENCES (23)
1.
Pega F, Momen NC, Streicher KN, et al. Global, regional and national burdens of non-melanoma skin cancer attributable to occupational exposure to solar ultraviolet radiation for 183 countries, 2000–2019: A systematic analysis from the WHO/ILO Joint Estimates of the Work-related Burden of Disease and Injury. Environ Int. 2023; 181: 108226. https://doi.org/10.1016/j.envi....
2.
Pellegrini S, Elefanti L, Dall'Olmo L, et al. The Interplay between Nevi and Melanoma Predisposition Unravels Nevi-Related and Nevi-Resistant Familial Melanoma. Genes (Basel). 2021;12(7):1077. https://doi:10.3390/genes12071....
3.
Loney T, Paulo MS, Modenese A, et al. Global evidence on occupational sun exposure and keratinocyte cancers: A systematic review. Br J Dermatol. 2021;184(2):208–218. https://doi.org/10.1111/bjd.19....
4.
Schmitt J, Haufe E, Trautmann F, et al. Occupational UV-exposure is a major risk factor for basal cell carcinoma: Results of the population-based case-control study FB-181. J Occup Environ Med. 2018;60(1):36–43. https://doi.org/10.1097/JOM.00....
5.
Park YJ, Kwon GH, Kim JO, et al. A retrospective study of changes in skin cancer characteristics over 11 years. Arch Craniofac Surg. 2020;21(2):87–89. https://doi.org/10.7181/acfs.2....
6.
Schmitt J, Haufe E, Trautmann F, et al. Is ultraviolet exposure acquired at work the most important risk factor for cutaneous squamous cell carcinoma? Results of the population-based case-control study FB-181. Br J Dermatol. 2018;178(2):462–472. https://doi.org/10.1111/bjd.15....
7.
Bauer A, Haufe E, Heinrich L, et al. Basal cell carcinoma risk and solar UV exposure in occupationally relevant anatomic sites: Do histological subtype, tumor localization and Fitzpatrick phototype play a role? A population-based case-control study. J Occup Med Toxicol. 2020;15(1):28. https://doi.org/10.1186/s12995....
8.
Kullavanijaya P, Lim HW. Photoprotection. J Am Acad Dermatol. 2005;52(6):937–58. https://doi:10.1016/j.jaad.200....
9.
Alfonso JH, Bauer A, Bensefa-Colas L, et al. Minimum standards on prevention, diagnosis and treatment of occupational and work-related skin diseases in Europe—Position paper of the COST Action StanDerm (TD 1206). J Eur Acad Dermatol Venereol. 2017;31(1):31–43. https://doi.org/10.1111/jdv.14....
10.
Modenese A, Korpinen L, Gobba F. Solar radiation exposure and outdoor work: An underestimated occupational risk. Int J Environ Res Public Health. 2018;15(5):1020. https://doi.org/10.3390/ijerph....
11.
Buckley D, McMonagle C. Melanoma in primary care: the role of the general practitioner. Ir J Med Sci. 2014;183(3):363–368. https://doi.org/10.1007/s11845....
12.
Jović M, Marinković M, Suđecki B, et al. Skin cancer: Primary, secondary, and tertiary prevention. Part II. Cancer Prev Res (Phila). 2023;16(4):251–260. https://doi.org/10.1158/1940-6....
13.
Sabzevari N, Qiblawi S, Norton SA, et al. Sunscreens: UV filters to protect us: Part 1: Changing regulations and choices for optimal sun protection. Int J Womens Dermatol. 2021;7(1):28–44. https://doi.org/10.1016/j.ijwd....
14.
Sieniawska D, Proszowska P, Madoń M, et al. Ultraviolet-Protective Clothing and Sunscreen: Sun-Protection for Healthy Skin. J Educ Health Sport. 2024;71:51237 https://doi.org/10.12775/JEHS.....
15.
Rocholl M, Ludewig M, John SM, et al. Outdoor workers' perceptions of skin cancer risk and attitudes to sun-protective measures: A qualitative study. J Occup Health. 2020;62(1):e12083. https://doi.org/10.1002/1348-9....
16.
Gambichler T, Laperre J, Hoffmann K. The European standard for sun- protective clothing: EN 13758. J Eur Acad Dermatol Venereol. 2006;20(2):125–30. doi:10.1111/j.1468-3083.2006.01401.x.
17.
Diehl K, Schneider S, Seuffert S, et al. Who Are the Nonusers of Sunscreen, and What Are Their Reasons? Development of a New Item Set. J Canc Educ. 2021;36:1045–1053. https://doi.org/10.1007/s13187....
18.
Saes-Silva E, Dumith SC. Non-use of sunscreen among adults and the elderly in southern Brazil. An Bras Dermatol. 2019;94:567–573. https://doi.org/10.1016/j.abd.....
19.
Garbe C, Buettner PG. Predictors of the use of sunscreen in dermatological patients in Central Europe. Prev Med. 2000;31:134–139. https://doi.org/10.1006/pmed.2....
20.
Symanzik C, John SM. Prevention of occupational skin cancer caused by solar ultraviolet radiation exposure: Recent achievements and perspectives. Dermato. 2024;4(2):46–59. https://doi.org/10.3390/dermat....
21.
Rogowski-Tylman M, Jankowski M, Matusiak Ł, et al. Internet users' awareness of skin cancer and attitude towards skin self-examination: a cross-sectional survey. Adv Clin Exp Med. 2015;24(6):1053–1061. https://doi.org/10.17219/acem/....
22.
Coroiu A, Moran C, Bergeron C, et al. Operationalization of skin self-examination in randomized controlled trials with individuals at increased risk for melanoma: A systematic review. Patient Educ Couns. 2020;103(5):1013–1026. https://doi.org/10.1016/j.pec.....
23.
Chang RC, Yen H, Heskett KM, et al. The role of health literacy in skin cancer preventative behavior and implications for intervention: a systematic review. J Prev. 2024;45(6):957–972. https://doi.org/10.1007/s10935....
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.