RESEARCH PAPER
Economic determinants of financial performance in a public outpatient healthcare facility - retrospective study of health services financed by the National Health Fund
1
The Independent Group of Public Ambulatory Care Institutions Warsaw-Ochota, -, Polska
2
Health Innovation Unit, SGH Warsaw School of Economics, Polska
3
Department of Neurosurgery, Faculty of Medicine and Dentistry, Warsaw Medical University, Polska
4
Department of Community Psychiatry, Medical University of Warsaw, Polska
Corresponding author
Andrzej Silczuk
Department of Community Psychiatry, Faculty of Health Sciences, Medical University of Warsaw, Poland
Department of Community Psychiatry, Faculty of Health Sciences, Medical University of Warsaw, Poland
KEYWORDS
TOPICS
ABSTRACT
Introduction:
The Polish health care system has recently faced major financial pressures, including post- pandemic recovery, high inflation, statutory wage increases for medical personnel, and repeated tariff adjustments by the National Health Fund (NHF). Outpatient providers are expected to take over more services from hospitals, yet evidence on their financial sustainability under current NHF financing remains limited.
Objective:
The aim of the study is to evaluate the operational profitability of a public outpatient provider in a semi-urban setting funded mainly through NHF contracts, and to assess revenue and cost trends, and key determinants of financial performance relevant to similar non-hospital providers
Material and methods:
A retrospective analysis of aggregated data from the provider’s Hospital Information System and Enterprise Resource Planning system was conducted for January 2021 - June 2025. Descriptive statistics were used to assess trends in revenues, costs, personnel expenditures, operating margins and NHF cost coverage, with personnel costs analyzed separately for employment-contract and contracted staff.
Results:
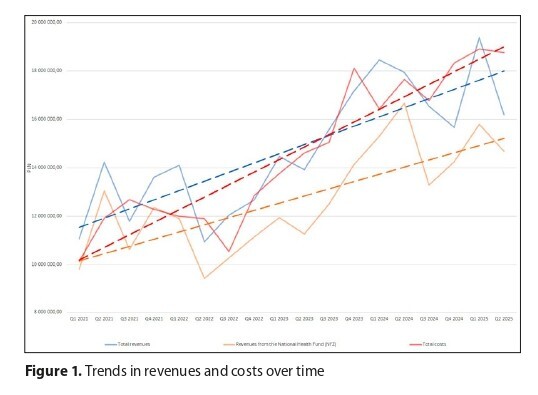
Revenues increased by 46%, NHF funding by 50% and total costs by 85%, with full cost coverage in only 20% of months. Personnel expenditures rose from 80% to over 86% of total costs. Average full time equivalent costs increased by 72% for employment-contract staff and by 233% for contracted personnel. From late 2022 onward, costs consistently exceeded revenues.
Conclusions:
The provider’s financial position deteriorated due to rapidly rising labour costs and insufficient NHF reimbursement adjustments. These trends indicate broader systemic pressures that may threaten the sustainability of publicly funded outpatient services unless tariff, wage and contracting policies are reformed.
The Polish health care system has recently faced major financial pressures, including post- pandemic recovery, high inflation, statutory wage increases for medical personnel, and repeated tariff adjustments by the National Health Fund (NHF). Outpatient providers are expected to take over more services from hospitals, yet evidence on their financial sustainability under current NHF financing remains limited.
Objective:
The aim of the study is to evaluate the operational profitability of a public outpatient provider in a semi-urban setting funded mainly through NHF contracts, and to assess revenue and cost trends, and key determinants of financial performance relevant to similar non-hospital providers
Material and methods:
A retrospective analysis of aggregated data from the provider’s Hospital Information System and Enterprise Resource Planning system was conducted for January 2021 - June 2025. Descriptive statistics were used to assess trends in revenues, costs, personnel expenditures, operating margins and NHF cost coverage, with personnel costs analyzed separately for employment-contract and contracted staff.
Results:
Revenues increased by 46%, NHF funding by 50% and total costs by 85%, with full cost coverage in only 20% of months. Personnel expenditures rose from 80% to over 86% of total costs. Average full time equivalent costs increased by 72% for employment-contract staff and by 233% for contracted personnel. From late 2022 onward, costs consistently exceeded revenues.
Conclusions:
The provider’s financial position deteriorated due to rapidly rising labour costs and insufficient NHF reimbursement adjustments. These trends indicate broader systemic pressures that may threaten the sustainability of publicly funded outpatient services unless tariff, wage and contracting policies are reformed.
REFERENCES (27)
1.
European Observatory on Health Systems and Policies. Poland: health system summary 2024. Copenhagen: WHO Regional Office for Europe; 2024. https://eurohealthobservatory.... (dostęp: 30.10.2025).
2.
OECD/European Observatory on Health Systems and Policies (2023), Poland: Country Health Profile 2023, State of Health in the EU, OECD Publishing, Paris, https://doi.org/10.1787/f597c8... https://www.oecd.org/en/public... (dostęp: 29.10.2025).
3.
Statistics Poland. Health care expenditure in 2021–2023. Warsaw: Statistics Poland; 2024. Available from: https://stat.gov.pl/en/topics/... (dostęp: 03.11.2025).
4.
Narodowy Fundusz Zdrowia. Pieniadze na zdrowie w 2025 r. NHF przygotowal projekt planu finansowego. Warsaw: NHF; 2024 Jul 1. https://www.NHF.gov.pl/aktualn... rojekt-planu-finansowego,8634.html (dostęp: 15.11.2025).
5.
Najwyzsza Izba Kontroli. Realizacja zadan przez Narodowy Fundusz Zdrowia w latach 2021–2024. Informacja o wynikach kontroli P/24/046. Warsaw: NIK; 2025. https://wartowiedziec.pl/attac... (dostęp: 30.10.2025).
6.
Dudek S, Kozlowski L, Wisniewski W. Finanse ochrony zdrowia pod scislym nadzorem procedury nadmiernego deficytu. Warsaw: Instytut Finansow Publicznych, Federacja Przedsiebiorcow Polskich; 2025. https://federacjaprzedsiebiorc... (dostęp: 15.11.2025).
7.
Maciuła-Ziomek A. Finanse NHF w oplacanym stanie. Rzadowi bedzie coraz trudniej zasypac deficyt. Interia Biznes. 2025 Feb 19 https://biznes.interia.pl/gosp... (dostęp: 30.10.2025).
8.
Kringos DS, Boerma WGW, Hutchinson A, et al., editors. Building primary care in a changing Europe: case studies. Copenhagen: European Observatory on Health Systems and Policies; 2015. https://www.ncbi.nlm.nih.gov/b... (dostęp: 30.10.2025).
9.
Busby J, Purdy S, Hollingworth W. A systematic review of the magnitude and cause of geographic variation in unplanned hospital admission rates and length of stay for ambulatory care sensitive conditions. BMC Health Serv Res. 2015; 15: 324.
10.
Becker NV, Karmakar M, Tipirneni R, Ayanian JZ. Trends in hospitalizations for ambulatory care sensitive conditions during the COVID 19 pandemic. JAMA Netw Open. 2022; 5(3): e222933.
11.
Starfield B. Primary care and specialty care: a role reversal? Med Educ. 2003;37(9):756–757.
12.
Marasovic Susnjara I, Mijakovic M, Jurcev Savicevic A. The influence of the COVID 19 pandemic on hospitalizations for ambulatory care sensitive conditions in Split Dalmatia County, Croatia. Medicina. 2024; 60(4): 523.
13.
Dubas Jakobczyk K, Kocot E, Koziel A, Skrzypczynska E. Financial performance of public hospitals: a cross sectional study among Polish providers. Int J Environ Res Public Health. 2020; 17(7): 21-88.
14.
Sielska A. Costs of Polish county hospitals: a behavioral panel function. PLoS One. 2022; 17(1): e0262646.
15.
Zarzadzenie nr 62/2025/DEF Prezesa Narodowego Funduszu Zdrowia z dnia 23 lipca 2025 r. w sprawie zmiany planu finansowego Narodowego Funduszu Zdrowia na 2025 rok. Warsaw: NHF; 2025. Available from: https://mbrk.pl/wp-content/upl... (dostęp: 10.11.2025).
16.
Brinster CJ, Escousse GT, Rivera PA, Sternbergh WC 3rd, Money SR. Drastic increase in hospital labor costs led to a sustained financial loss for an academic vascular surgery division during the coronavirus disease 2019 pandemic. J Vasc Surg. 2022 Dec; 76(6): 1710-1718. doi: 10.1016/j.jvs.2022.07.004.
17.
Beauvais B, Richter JP, Strowd B, et al. An exploratory analysis of the association between hospital labor costs and financial performance. Inquiry. 2023;60:1–10.
18.
American Hospital Association. Costs of caring: the rising cost of caring for patients and communities. AHA; 2025. https://www.aha.org/costsofcar... (dostęp: 10.11.2025).
19.
Korneta P. Medical staff shortages and the performance of outpatient clinics in Poland during the COVID-19 pandemic. Zeszyty Naukowe PW; 2022. https://repo.pw.edu.pl/docstor... (dostęp: 10.11.2025).
20.
Korneta P. The impact of the COVID-19 pandemic on the financial and quality performance of primary health care providers in Poland. Health Policy. 2021. https://repo.pw.edu.pl/docstor... (dostęp: 10.11.2025).
21.
Wagenschieber E, Blunck D. Impact of reimbursement systems on patient care - a systematic review of systematic reviews. Health Econ Rev. 2024 Mar 16;14(1):22. doi: 10.1186/s13561-024-00487-6.
22.
OECD. Better ways to pay for health care. Paris: OECD Publishing; 2025 update. https://www.oecd.org/content/d... OECD (dostęp: 12.11.2025).
23.
Cappuccio S, Li Y, Song C, Liu E, Glaser G, Casarin J, Grassi T, Butler K, Magtibay P, Magrina JF, Scambia G, Mariani A, Langstraat C. The shift from inpatient to outpatient hysterectomy for endometrial cancer in the United States: trends, enabling factors, cost, and safety. Int J Gynecol Cancer. 2021 May;31(5):686-693. doi: 10.1136/ijgc-2020-002192.
24.
Zhao Y, et al. Substituting inpatient for outpatient care: impact on hospital costs and efficiency. Health Policy. 2024. https://www.researchgate.net/p... (dostęp: 03.11.2025).
25.
Rieder L, Thomet C, von Eiff W, et al. Strategies for successful hospital-based outpatient care: expert perspectives from Switzerland and Germany. Health Syst. 2025;2(2):1–18.
26.
OECD. Trends in the financialisation of outpatient care across OECD countries. Paris: OECD Publishing; 2025. https://www.oecd.org/content/d... (dostęp: 10.11.2025).
27.
Mularczyk-Tomczewska P, Gujski M, Koperdowska JM, et al. Factors Influencing Patient Satisfaction with Healthcare Services in Poland. Med Sci Monit. 2025 Jun 19;31:e948225. doi: 10.12659/MSM.948225.
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.