RESEARCH PAPER
Evaluation of the effect of liraglutide therapy on body weight and insulin resistance.
1
National Medical Institute of the Ministry of the Interior and Administration, Warsaw, Poland
Corresponding author
Waldemar Wierzba
National Medical Institute of the Ministry of the Interior and Administration, Warsaw, Poland
National Medical Institute of the Ministry of the Interior and Administration, Warsaw, Poland
Med Og Nauk Zdr. 2023;29(4):290-292
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Insulin resistance is a state of reduced tissue sensitivity to insulin action despite normal or elevated serum insulin levels. Liraglutide (a GLP-1 receptor agonist) stimulates insulin secretion from the pancreas while decreasing excessive glucagon release. GLP-1 analogues have a unique beneficial effect on weight loss by stimulating insulin secretion without increasing blood sugar levels excessively. The aim of the study was to investigate the effects of liraglutide on body mass index and insulin resistance in overweight and obese non-diabetic individuals.
Material and methods:
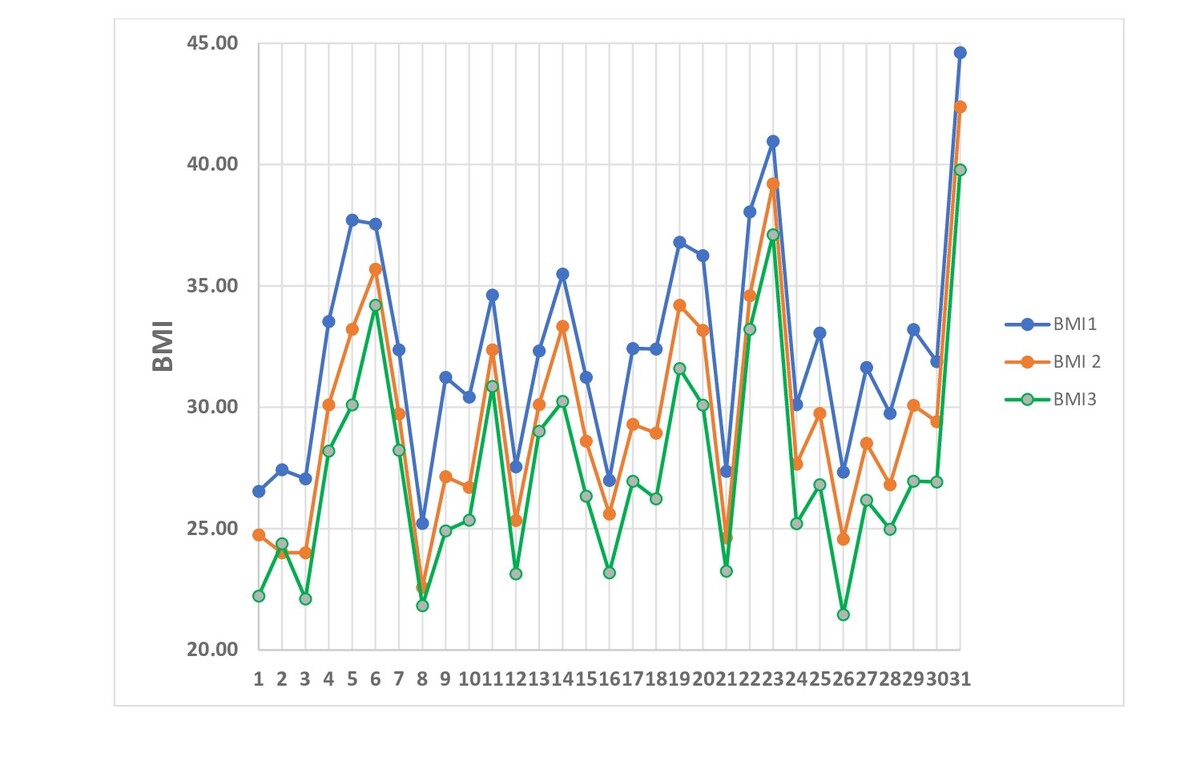
The study involved 31 overweight and obese women (BMI of ≥25 kg/m2) who received liraglutide treatment between 2021–2022. Liraglutide 3.0 mg was used as an adjunct to behavioural therapy, which included a lowcalorie diet and exercise programme. The study collected BMI, glucose and insulin levels, and HOMA index before and during liraglutide treatment. Body weight and blood tests were examined at baseline (BMI1, HOMA1), as well as at 3 (BMI2, HOMA2), and 6 months (BMI3, HOMA3) of treatment to observe any changes.
Results:
Average age of participants – 38.32±7.41 years. Changes in BMI from baseline (32.36±4.56 kg/m²) to 6 months (27.46±4.45kg/m²) were associated with a significant reduction in weight (p <0.001). Changes in HOMA index from baseline (4.73±1.48) to 3 (3.59±1.26) and 6 months (2.47±0.91) were statistically significant (p <0.03, p < 0.001).
Conclusions:
Liraglutide represents a promising option for reducing body weight and obesity in non-diabetic patients as an adjunct to behavioural therapy. Agonists GLP-1 receptor, representing a new class of antidiabetic drug, undoubtedly offer unique benefits for overweight or obesity patients. Liraglutide in 3.0 mg use was associated with a significant weight reduction and lowering of insulin resistance.
Insulin resistance is a state of reduced tissue sensitivity to insulin action despite normal or elevated serum insulin levels. Liraglutide (a GLP-1 receptor agonist) stimulates insulin secretion from the pancreas while decreasing excessive glucagon release. GLP-1 analogues have a unique beneficial effect on weight loss by stimulating insulin secretion without increasing blood sugar levels excessively. The aim of the study was to investigate the effects of liraglutide on body mass index and insulin resistance in overweight and obese non-diabetic individuals.
Material and methods:
The study involved 31 overweight and obese women (BMI of ≥25 kg/m2) who received liraglutide treatment between 2021–2022. Liraglutide 3.0 mg was used as an adjunct to behavioural therapy, which included a lowcalorie diet and exercise programme. The study collected BMI, glucose and insulin levels, and HOMA index before and during liraglutide treatment. Body weight and blood tests were examined at baseline (BMI1, HOMA1), as well as at 3 (BMI2, HOMA2), and 6 months (BMI3, HOMA3) of treatment to observe any changes.
Results:
Average age of participants – 38.32±7.41 years. Changes in BMI from baseline (32.36±4.56 kg/m²) to 6 months (27.46±4.45kg/m²) were associated with a significant reduction in weight (p <0.001). Changes in HOMA index from baseline (4.73±1.48) to 3 (3.59±1.26) and 6 months (2.47±0.91) were statistically significant (p <0.03, p < 0.001).
Conclusions:
Liraglutide represents a promising option for reducing body weight and obesity in non-diabetic patients as an adjunct to behavioural therapy. Agonists GLP-1 receptor, representing a new class of antidiabetic drug, undoubtedly offer unique benefits for overweight or obesity patients. Liraglutide in 3.0 mg use was associated with a significant weight reduction and lowering of insulin resistance.
ABBREVIATIONS
Abbreviations
BMI – Body Mass Index; HOMA – Homeostasis Model
Assessment – Insulin Resistance; GLP-1 – Glucagon-Like
Peptide-1
REFERENCES (12)
1.
Szydlarska D, Machaj M, Jakimiuk A. History of discovery of polycystic ovary syndrome. AdvClinExp Med. 2017 May Jun;26(3):555–558.
2.
Shin-Hae L, Shi-Young P, Cheol SC. Insulin Resistance: From Mechanism to Therapeutic Strategies. DiabetesMetab J. 2022 Jan;46(1):15–37.
3.
Donna H, Ryan S, Ryan Y. Weight Loss and Improvement in Comorbidity: Differences at 5%, 10%, 15%, and Over. CurrObes Rep. 2017 Jun;6(2):187–194.
4.
Bray GA, Heisel WE, Afshin A, et al. The Science of Obesity Management: An Endocrine Society Scientific Statement. Endocr Rev. 2018 Apr;39(2):79–132.
5.
Overgaard RV, Petri KC, Lisbeth V, et al. Liraglutide 3.0 mg for Weight Management: A Population Pharmacokinetic Analysis. Clin Pharmacokinet. 2016;55(11):1413–1422.
6.
Pei Zhang, Yu Liu, Yuan Ren, Jie Bai, et al. The efficacy and safety of liraglutide in the obese, non-diabetic individuals: a systemic review and meta-analysis. Afr Health Sci. 2019 Sep;19(3):2591–2599.
7.
Garber AJ, Henry R, Ratner R, et al. Liraglutide versus glimepiride monotherapy for type 2 diabetes (lead-3 mono): a randomised, 52-week, phase iii, double-blind, parallel-treatment trial. Lancet, 2009;373:473–481.
8.
Astrup A, Rossner S, Van Gaal L, et al. Effects of Liraglutide in the treatment of obesity: a randomised, double-blind, placebo-controlled study. Lancet. 2009;374:1606–1616.
9.
Sharma A, Ambrosy AP, DeVore AD, et al. Liraglutide and weight loss among patients with advanced heart failure and a reducedejection fraction: insights from the FIGHT trial. ESC Heart Fail. 2018 Dec;5(6):1035–1043.
10.
Garvey WT, Birkenfeld AL, Dicker D, Mingrone G, et al. Efficacy and Safety of Liraglutide 3.0 mg in Individuals With Overweight or Obesity and Type 2 Diabetes Treated With Basal Insulin: The SCALE Insulin Randomized Controlled Trial. Diabetes Care. 2020 May;43(5):1085–1093.
11.
Kadouh H, Chedid V, Halawi H, et al. GLP-1 Analog Modulates Appetite, Taste Preference, Gut Hormones, and Regional Body Fat Stores in Adults with Obesity. J Clin Endocrinol Metab. 2020; 105(5): 1552–1563.
12.
Cosentino F, Ceriello A, Baeres FMM, et al. Addressing cardiovascular risk in type 2 diabetes mellitus: a report from the European Society of Cardiology Cardiovascular Roundtable. Eur Heart J. 2019 Sep 7;40(34):2907–2919.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.