REVIEW PAPER
Metabolic disorders and other diseases among shift workers – a review of current research
1
Warszawski Uniwersytet Medyczny, Warszawa, Polska, Wydział Lekarski, Zakład Medycyny Społecznej i Zdrowia Publicznego, Polska
2
Studenckie Koło Naukowe Higieny i Profilaktyki, Warszawski Uniwersytet Medyczny, Warszawa, Polska, Wydział Lekarski, Zakład Medycyny Społecznej i Zdrowia Publicznego, Polska
Corresponding author
Aleksandra Kozłowska
Warszawski Uniwersytet Medyczny, Warszawa, Polska, Wydział Lekarski, Zakład Medycyny Społecznej i Zdrowia Publicznego, ul. Oczki 3, 02–007, Warszawa, Polska
Warszawski Uniwersytet Medyczny, Warszawa, Polska, Wydział Lekarski, Zakład Medycyny Społecznej i Zdrowia Publicznego, ul. Oczki 3, 02–007, Warszawa, Polska
Med Og Nauk Zdr. 2022;28(1):40-47
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
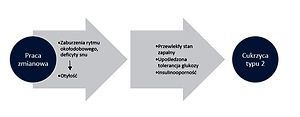
Shift work has a number of negative effects on human health. It often leads to sleep deprivation, changes of circadian rhythm, level of physical activity and eating habits, and also increases the risk of development of metabolic disorders and gastrointestinal diseases. The aim of the study was to indicate and discuss the most common metabolic disorders and other gastrointestinal pathologies in the context of data from literature concerning shift workers.
Review methods:
The effect of shift work on metabolic disorders in shift workers was assessed by searching reports from the last 10 years in the Medline database (http://www. ncbi.nlm.nih.gov/pubmed)
Brief description of the state of knowledge:
Numerous observations of shift workers unequivocally showed an increased risk of overweight, obesity and metabolic syndrome among this group. Increased waist circumference was characteristic of people working in this employment system in relation to units working only during the day. Many authors emphasized that there is a correlation between shift work and the risk of type 2 diabetes. Moreover, the risk of developing this disease was 9% higher in shift workers. It was found that sleep deprivation, which is typical of shift workers, may increase the level of glycated haemoglobin, HbA1c, and increase the risk of prediabetes. In addition, it is emphasized that sleep disorders occurring in shift workers also contribute to the development or aggravation of reflux disease.
Summary:
The authors highlighted the need for introduction of multidirectional preventive measures among shift workers in order to reduce the negative effect of shift work on humanhealth. In terms of public health, taking into account the type of work performed is an important element of patient care in the field of professional practice of either occupational medicine physicians or general practitioners.
Shift work has a number of negative effects on human health. It often leads to sleep deprivation, changes of circadian rhythm, level of physical activity and eating habits, and also increases the risk of development of metabolic disorders and gastrointestinal diseases. The aim of the study was to indicate and discuss the most common metabolic disorders and other gastrointestinal pathologies in the context of data from literature concerning shift workers.
Review methods:
The effect of shift work on metabolic disorders in shift workers was assessed by searching reports from the last 10 years in the Medline database (http://www. ncbi.nlm.nih.gov/pubmed)
Brief description of the state of knowledge:
Numerous observations of shift workers unequivocally showed an increased risk of overweight, obesity and metabolic syndrome among this group. Increased waist circumference was characteristic of people working in this employment system in relation to units working only during the day. Many authors emphasized that there is a correlation between shift work and the risk of type 2 diabetes. Moreover, the risk of developing this disease was 9% higher in shift workers. It was found that sleep deprivation, which is typical of shift workers, may increase the level of glycated haemoglobin, HbA1c, and increase the risk of prediabetes. In addition, it is emphasized that sleep disorders occurring in shift workers also contribute to the development or aggravation of reflux disease.
Summary:
The authors highlighted the need for introduction of multidirectional preventive measures among shift workers in order to reduce the negative effect of shift work on humanhealth. In terms of public health, taking into account the type of work performed is an important element of patient care in the field of professional practice of either occupational medicine physicians or general practitioners.
REFERENCES (73)
1.
Cox KH, Takahashi JS. Circadian clock genes and the transcriptional architecture of the clock mechanism. J Mol Endocrinol. 2019; 63(4): 93–102. https://doi.org/10.1530/JME-19....
2.
Poggiogalle E, Jamshed H, Peterson CM. Circadian regulation of glucose, lipid, and energy metabolism in humans. Metabolism. 2018 Jul; 84: 11–27. doi: 10.1016/j.metabol.2017.11.017.
3.
Pot GK. Sleep and dietary habits in the urban environment: the role of chrono-nutrition. Proc Nutr Soc. 2018 Aug; 77(3): 189–198. doi: 10.1017/S0029665117003974.
4.
Brum MCB, Dantas FF, Schnorr CC, et al. Shift work and its association with metabolic disorders. Diabetol Metab Syndr. 2015; 7(1): 45. https://doi.org/10.1186/s13098....
5.
Wołyniec W, Kurlapski M, Januszczyk J, et al. Cukrzyca w społeczeństwie 24/7. Związek między pracą zmianową a zaburzeniami metabolicznymi. Diabetol Klin. 2015; 4(1): 22–28.
6.
Li Y, Ma J, Yao K, et al. Circadian rhythms and obesity: Timekeeping governs lipid metabolism. J Pineal Res. 2020; 69(3): 12682. https://doi.org/ 10.1111/jpi.12682.
7.
Cheng P, Drake C. Shift Work Disorder. Neurol Clin. 2019; 37(3): 563–577. https://doi.org/ 10.1016/j.ncl.2019.03.003.
8.
Directive 2000/34/EC of the European Parliament and of the Council of 22 June 2000 amending Council Directive93/104/EC concerning certain aspects of the Organization of working time to cover sectors and activities excluded from that Directive. Official Journal: 195,01/08/2000.
9.
Jang TW. Work-Fitness Evaluation for Shift Work Disorder. Int J Environ Res Public Health. 2021; 18(3): 1294. https://doi.org/10.3390/ijerph....
10.
Obwieszczenie Marszałka Sejmu Rzeczpospolitej Polskiej z dnia 8 września 2016 r. w sprawie ogłoszenia jednolitego tekstu ustawy- Kodeks Pracy. DzU z 2018 r., poz. 128.
11.
Blüher M. Obesity: global epidemiology and pathogenesis. Nat Rev Endocrinol. 2019; 15(5): 288–298. https://doi.org/10.1038/s41574....
12.
Kłosiewicz-Latoszek L. Otyłość jako problem społeczny, zdrowotny i leczniczy. Probl Hig Epidemiol. 2010; 91(3): 339–343.
13.
World Health Organization [Internet]. Organization, Genewa 2017 [cytowany 29 kwietnia 2019]. http://www.who.int/en/news-roo....
14.
Zgliczyński WS. Nadwaga i otyłość w Polsce. Warszawa: Infos. Wydawnictwo Sejmowe dla Biura Analiz Sejmowych; 2017.
15.
Qin P, Li Q, Zhao Y, et al. Sugar and artificially sweetened beverages and risk of obesity, type 2 diabetes mellitus, hypertension, and all-cause mortality: a dose-response meta-analysis of prospective cohort studies. Eur J Epidemiol. 2020; 35(7): 655–671. https://doi.org/ 10.1007/s10654-020-00655-y.
16.
Davies A, Wellard-Cole L, Rangan A, et al. Validity of self-reported weight and height for BMI classification: A cross-sectional study among young adults. Nutrition. 2020; 71: 110622. https://doi.org/10.1016/j.nut.....
17.
Geliebter A, Gluck ME, Tanowitz M, et al. Work-shift period and weight change. Nutrition. 2000; 16(1): 27–29. https://doi.org/10.1016/S0899-....
18.
Burdelak W, Pepłońska B. Praca w nocy a zdrowie pielęgniarek i położnych – przegląd literatury. Med Pr. 2013; 64(3): 397–418.
19.
Copertaro A, Bracci M, Barbaresi M, et al. Assessment of cardiovascular risk in shift healthcare workers. Eur J Cardiovasc Prev Rehabil. 2008; 15(2): 224–229. https://doi.org/10.1097/HJR.0b....
20.
Zhang Q, Chair SY, Lo SHS, et al. Association between shift work and obesity among nurses: A systematic review and meta-analysis. Int J Nurs Stud. 2020; 112: 103757. https://doi.org/10.1016/j.ijnu....
21.
da Silva JC, Garcez A, Cibeira GH, et al. Relationship of work-related stress with obesity among Brazilian female shift workers. Public Health Nutr. 2021; 24(2): 260–266. https://doi.org/doi: 10.1017/S1368980020004243.
22.
Niedhammer I, Lert F, Marne M. Prevalence of overweight and weight gain in relation to night work in a nurses› cohort. Int J Obes Relat Metab Disord. 1996; 20(7): 625–633.
23.
Marquezea EC, Lemosa LC, Soaresa N, et al. Weight gain in relation to night work among nurses. Work. 2012; 41: 2043–2048. https://doi.org/10.3233/WOR-20....
24.
Barbadoro P, Santarelli L, Croce N, et al. Rotating shift-work as an independent risk factor for overweight Italian workers: a cross-sectional study. PLoS One. 2013; 8(5): e63289. https://doi.org/10.1371/journa....
25.
Son M, Ye BJ, Kim J-I, et al. Association between shift work and obesity according to body fat percentage in Korean. Ann Occup Environ Med. 2015; 27: 1–9. https://doi.org/10.1186/s40557....
26.
Mcglynn N, Kirsh VA, Cotterchio M, et al. Shift work and obesity among Canadian women: a cross-sectional study using a novel exposure assessment tool. PloS One. 2015; 10(9): e0137561. https://doi.org/10.1371/journa....
27.
Peplonska B, Bukowska A, Sobala W. Association of rotating night shift work with BMI and abdominal obesity among nurses and midwives. PLoS One. 2015; 10(7): e0133761. https://doi.org/10.1371/journa....
28.
Sun M, Feng W, Wang F, et al. Meta-analysis on shift work and risks of specific obesity types. Obes Rev. 2018; 19(1): 28–40. https://doi.org/10.1111/obr.12....
29.
Bysiak D, Sosna A, Zielińska K. Ocena wyrównania metabolicznego u chorych na cukrzycę typu 2 pracujących w systemie zmianowym. Clin Diabetol. 2015; 4(4): 132–40. https://doi.org/10.5603/DK.201....
30.
Cole JB, Florez JC. Genetics of diabetes mellitus and diabetes complications. Nat Rev Nephrol. 2020; 16(7): 377–390. https://doi.org/10.1038/s41581....
31.
Gan Y, Yang C, Tong X, et al. Shift work and diabetes mellitus: a meta-analysis of observational studies. Occup Environ Med. 2015; 72(1): 72–78. https://doi.org/ 10.1136/oemed-2014-102150.
32.
Kroenke CH, Spiegelman D, Manson J. et al. Work characteristics and incidence of type 2 diabetes in women. Am J Epidol. 2006; 165(2): 175–183. https://doi.org/10.1093/aje/kw....
33.
Kuleta A. Wpływ pracy zmianowej na wystąpienie zmian patofizjologicznych—przegląd literatury. Forum Zab Metabol. 2016; 7(2): 93–98.
34.
Wei YQ, Ma AJ, Fang K. Association between sleep and serum hemoglobin A1c in nondiabetic population in Beijing. 2020; 41(8): 1256–1260. https://doi.org/ 10.3760/cma.j.cn112338-20191224-00911.
35.
Bener A, Al-Hamaq AOAA, Agan AF, et al. Sleeping disturbances and predictor risk factors among type 2 diabetic mellitus patients. Ann Afr Med. 2020; 19(4): 230–236. https://doi.org/10.4103/aam.aa....
36.
Oosterman JE, Wopereis S, Kalsbeek A. The Circadian Clock, Shift Work, and Tissue-Specific Insulin Resistance. Endocrinology. 2020; 161(12): 1–11. https://doi.org/ 10.1210/endocr/bqaa180.
37.
Jarosz M, Bułhak-Jachymczyk B. Normy żywienia człowieka. Wydawnictwo Lekarskie, Warszawa 2008.
38.
Vetter C, Dashti HS, Lane JM, et al. Night shift work, genetic risk, and type 2 diabetes in the UK Biobank. Diab Care. 2018; 41(4): 762–769. https://doi.org/10.2337/dc17-1....
39.
Hansen AB, Stayner L, Hansen J, et al. Night shift work and incidence of diabetes in the Danish Nurse Cohort. Occup Environ Med. 2016; 73(4): 262–268. https://doi.org/10.1136/oemed-....
40.
Wyrzykowski B, Zdrojewski T, Sygnowska E, et al. Epidemiologia zespołu metabolicznego w Polsce. Wyniki programu WOBASZ. Kardiol Pol. 2005; 63(4): 1–4.
41.
Salska A, Chiżyński K, Salski W, et al. Choroby układu krążenia związane z pracą zawodową— istotny problem zdrowotny osób pracujących. Chor Serca Nacz. 2015; 12(2): 75–87.
42.
Punthakee Z, Goldenberg R, Katz P. Definition, Classification and Diagnosis of Diabetes, Prediabetes and Metabolic Syndrome. Can J Diabetes. 2018; 42: 10–15. https://doi.org/10.1016/j.jcjd....
43.
Ninomiya JK, L’Italien G, Criqui MH, et al. Association of the metabolic syndrome with history of myocardial infarction and stroke in the Third National Health and Nutrition Examination Survey. Circulation. 2004; 109(1): 42–46. https://doi.org/10.1161/01.CIR....
44.
Kawabe Y, Nakamura Y, Kikuchi S, et al. Relationship between shift work and clustering of the metabolic syndrome diagnostic components. J Atheroscler Thromb. 2014; 21(7): 703–711. https://doi.org/10.5551/jat.19....
45.
Guo Y, Rong Y, Huang X, et al. Shift work and the relationship with metabolic syndrome in Chinese aged workers. PLoS One. 2015; 10(3): 1–12. https://doi.org/10.1371/journa....
46.
Sohail S, Yu L, Bennett DA, et al. Irregular 24-hour activity rhythms and the metabolic syndrome in older adults. Chronobiol Int. 2015; 32(6): 802–813. https://doi.org/10.3109/074205....
47.
Wojtyniak B, Goryński P, Moskalewicz B. Sytuacja zdrowotna ludności Polski i jej uwarunkowania. J Oncolo. 2013; 63(3): 269.
48.
Townsend N, Wilson L, Bhatnagar P, et al. Cardiovascular disease in Europe: epidemiological update 2016. Eur Heart J. 2016; 37(42): 3232–3245. https://doi.org/ 10.1093/eurheartj/ehw334.
49.
Uchmanowicz I, Hoes A, Perk J, et al. Optimising implementation of European guidelines on cardiovascular disease prevention in clinical practice: what is needed? Eur J Prev Cardiol. 2020;3: 2047487320926776. https://doi.org/10.1177/204748....
50.
Pawlak J, Pawlak B, Zalewski P. Praca zmianowa a powstawanie chorób układu sercowo-naczyniowego w kontekście regulacji normatywnej. Hyg Publ Health. 2013; 48(1): 6–9.
51.
Pimenta AM, Kac G, Campos RR, et al. Night-shift work and cardiovascular risk among employees of a public university. Rev Assoc Med Brasil. 2012; 58(2): 168–177. https://doi.org/10.1590/S0104-....
52.
Brown DL, Feskanich D, Sánchez BN, et al. Rotating night shift work and the risk of ischemic stroke. Am J Epidemiol. 2009; 169(11): 1370–1377. https://doi.org/10.1093/aje/kw....
53.
Gangwisch JE, Feskanich D, Malaspina D, et al. Sleep duration and risk for hypertension in women: results from the nurses’ health study. Am J Hypertens. 2013; 26(7): 903–911. https://doi.org/10.1093/ajh/hp....
54.
Yeom JH, Sim CS, Lee J, et al. Effect of shift work on hypertension: cross sectional study. Ann Occup Environ Med. 2017; 29(1): 11. https://doi.org/10.1186/s40557....
55.
Ceïde ME, Pandey A, Ravenell J, et al. Associations of short sleep and shift work status with hypertension among Black and White Americans. Int J Hypertens. 2015: 1–7. https://doi.org/10.1155/2015/6....
56.
Holmer BJ, Lapierre SS, Jake-Schoffman DE, et al. Effects of sleep deprivation on endothelial function in adult humans: a systematic review. Geroscience. 2021; 43(1): 137–158. https://doi.org/10.1007/s11357....
57.
Kaźmierczak A, Lewandowski J, Artyszuk Ł. Wpływ melatoniny na profil dobowy ciśnienia u chorych z brakiem nocnego obniżenia ciśnienia tętniczego. Arter Hypertens. 2014; 18(3): 134–142.
58.
Saberi HR, Moravveji AR. Gastrointestinal complaints in shift-working and day-working nurses in Iran. J Circadian Rhythms. 2010; 8(1): 9. https://doi.org/10.1186/1740-3....
59.
Segawa K, Nakazawa S, Tsukamoto Y, et al. Peptic ulcer is prevalent among shift workers. Dig Dis Sci. 1987; 32(5): 449–453. https://doi. org/10.1007/BF01296025.
60.
Knutsson A, Bøggild H. Gastrointestinal disorders among shift workers. Scand J Work Environ Health. 2010: 85–95. https://doi.org/10.5271/ sjweh.2897.
61.
Lin HY, Weng SF, Lin HJ, et al. Peptic ulcer disease in healthcare workers: a nationwide population-based cohort study. PLoS One. 2015; 10(8): 0135456. https://doi.org/10.1371/journa....
62.
Lee S, Chae CH, Park C, et al. Relationship of shift work with endoscopic gastritis among workers of an electronics company. Scand J Work Environ Health. 2020; 46(2): 161–167. https://doi.org/10.5271/sjweh.....
63.
Clarrett DM, Hachem C. Gastroesophageal Reflux Disease (GERD). Mo Med. 2018; 115(3): 214–218.
64.
Kellerman R, Kintanar T. Gastroesophageal Reflux Disease. Prim Care. 2017; 44(4): 561–573. https://doi.org/10.101 /j.pop.2017.07.001.
65.
Yamamichi N, Mochizuki S, Asada-Hirayama I, et al. Lifestyle factors affecting gastroesophageal reflux disease symptoms: a cross-sectional study of healthy 19864 adults using FSSG scores. BMC Med. 2012; 10(1): https://doi.org/10.1186/1741–7....
66.
Xue J, Zhao Y, Wang Z, et al. Rotating night shift work is associated with an increased risk of gastroesophageal reflux disease (GERD) symptoms among workers in China: A cross-sectional study. Int J Clin Pract. 2021; 75(4): e13848. https://doi.org/10.1111/ijcp.1....
67.
Enck P, Azpiroz F, Boeckxstaens G, et al. Functional dyspepsia. Nat Rev Dis Primers. 2017; 3: 17081. https://doi.org/10.103 /nrdp.2017.81.
68.
Ng QX, Soh AYS, Loke W, et al. The role of inflammation in irritable bowel syndrome (IBS). J Inflamm Res. 2018; 21(11): 345–349. https:// doi.org/ 10.2147/JIR.S174982.
69.
Huang ZP, Li SM, Shen T, et al. Correlation between sleep impairment and functional dyspepsia. J Int Med Res. 2020; 48(7): 300060520937164. https://doi.org/ 10.1177/0300060520937164.
70.
Kim HI, Jung S, Choi JY, et al. Impact of shiftwork on irritable bowel syndrome and functional dyspepsia. J Korean Med Sci. 2013; 28(3): 431–437. https://doi.org/10.3346/jkms.2....
71.
Nojkov B, Rubenstein JH, Chey WD, et al. The impact of rotating shift work on the prevalence of irritable bowel syndrome in nurses. Am J Gastroenterol. 2010; 105(4): 842–847. https://doi.org/10.1038/ajg.20....
72.
Lu WZ, Gwee KA, Ho KY. Functional bowel disorders in rotating shift nurses may be related to sleep disturbances. Europ J Gastroenterol Hepatol. 2006; 18(6): 623–627. https://doi.org/10.1097/000427...- 200606000-00008.
73.
Martchenko A, Martchenko SE, Biancolin AD, et al. Circadian Rhythms and the Gastrointestinal Tract: Relationship to Metabolism and Gut Hormones. Endocrinology. 2020; 161(12): bqaa167. https://doi. org/10.1210/endocr/bqaa167.™.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.