Online first
Bieżący numer
Archiwum
O czasopiśmie
Polityka etyki publikacyjnej
System antyplagiatowy
Instrukcje dla Autorów
Instrukcje dla Recenzentów
Rada Redakcyjna
Komitet Redakcyjny
Recenzenci
Wszyscy recenzenci
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
Kontakt
Bazy indeksacyjne
Klauzula przetwarzania danych osobowych (RODO)
PRACA PRZEGLĄDOWA
Kompleksowy przegląd wpływu mikroplastików na układ oddechowy, pokarmowy i moczowy – mechanizmy toksyczności i implikacje zdrowotne
1
Clinic of Cardiology and Internal Diseases, 5th Military Clinical Hospital with Polyclinic SPZOZ, Kraków, Poland
2
Department of Internal Diseases and Diabetology, Regional Hospital, Bielsko-Biała, Poland
3
Department of Internal Diseases, Ludwik Rydygier Specialized Hospital, Kraków, Poland
4
Department of Internal Diseases I, Regional Hospital, Kielce, Poland
5
Department of Internal Diseases, Specialized Hospital named after Dr. Tytus Chałubiński, Radom, Poland
Zaznaczeni autorzy mieli równy wkład w przygotowanie tego artykułu
Autor do korespondencji
Monika Domagała
Clinic of Cardiology and Internal Diseases, 5th Military Clinical Hospital with Polyclinic SPZOZ, Kraków, Polska
Clinic of Cardiology and Internal Diseases, 5th Military Clinical Hospital with Polyclinic SPZOZ, Kraków, Polska
Med Og Nauk Zdr. 2025;31(3):149-155
SŁOWA KLUCZOWE
mikroplastiknanoplastikzanieczyszczenia środowiskowetoksyczność mikroplastikuchoroby nerekchoroby układu oddechowego
DZIEDZINY
STRESZCZENIE
Wprowadzenie i cel:
Globalna produkcja plastiku w 2021 roku wynosiła 390,7 mln ton i liczba ta rokrocznie się zwiększa. Akumulację cząsteczek mikroplastiku (MP) zaobserwowano we wszystkich tkankach i płynach ustrojowych, a szczególnie narażone na jego toksyczne działanie – ze względu na bezpośredni kontakt z MP – są drogi oddechowe, przewód pokarmowy i układ moczowy
Metody przeglądu:
W celu przeprowadzenia przeglądu literatury przeszukano bazę PubMed przy użyciu różnych kombinacji konkretnych haseł: „microplastics”, „nanoplastics”, „lung diseases”, „intestinal diseases”, „renal diseases” i „hepatic diseases”.
Opis stanu wiedzy:
odpowiedzi na stymulację mikroplastikiem w miąższu płucnym zaobserwowano zaburzenia równowagi stresu oksydacyjnego i wzrost powstawania wolnych rodników, rozwój zapalenia poprzez aktywację szlaku NF-κB zależnego od fosforylacji p38 oraz szlaku Wnt/β-katenina. Podobne zmiany dostrzeżono w przewodzie pokarmowym, gdzie z powodu aktywacji przez mikroplastik szlaku zależnego od stresu oksydacyjnego ROS–NF-κB/NLRP3/IL-1β/MLCK dochodziło do uszkodzenia bariery jelitowej oraz zaburzeń w składzie, a także w metabolizmie mikrobioty. W miąższu nerki pod wpływem działania MP oprócz aktywacji wspomnianych wyżej mechanizmów zapalnych wykazano również zahamowanie proliferacji komórek, gromadzenie się mikroplastiku w ich wnętrzu oraz spadek ekspresji genów kodujących enzymy antyoksydacyjne, co zmniejszało zdolność komórek do neutralizowania wolnych rodników i nasilało efekt cytotoksyczny.
Podsumowanie:
Codzienna ekspozycja na mikroplastiki wymaga rzetelnej oceny zagrożenia poprzez interdyscyplinarne badania oparte na realistycznych stężeniach środowiskowych, uwzględniające długoterminowe skutki, właściwości fizykochemiczne cząstek oraz ich oddziaływania z innymi substancjami.
Globalna produkcja plastiku w 2021 roku wynosiła 390,7 mln ton i liczba ta rokrocznie się zwiększa. Akumulację cząsteczek mikroplastiku (MP) zaobserwowano we wszystkich tkankach i płynach ustrojowych, a szczególnie narażone na jego toksyczne działanie – ze względu na bezpośredni kontakt z MP – są drogi oddechowe, przewód pokarmowy i układ moczowy
Metody przeglądu:
W celu przeprowadzenia przeglądu literatury przeszukano bazę PubMed przy użyciu różnych kombinacji konkretnych haseł: „microplastics”, „nanoplastics”, „lung diseases”, „intestinal diseases”, „renal diseases” i „hepatic diseases”.
Opis stanu wiedzy:
odpowiedzi na stymulację mikroplastikiem w miąższu płucnym zaobserwowano zaburzenia równowagi stresu oksydacyjnego i wzrost powstawania wolnych rodników, rozwój zapalenia poprzez aktywację szlaku NF-κB zależnego od fosforylacji p38 oraz szlaku Wnt/β-katenina. Podobne zmiany dostrzeżono w przewodzie pokarmowym, gdzie z powodu aktywacji przez mikroplastik szlaku zależnego od stresu oksydacyjnego ROS–NF-κB/NLRP3/IL-1β/MLCK dochodziło do uszkodzenia bariery jelitowej oraz zaburzeń w składzie, a także w metabolizmie mikrobioty. W miąższu nerki pod wpływem działania MP oprócz aktywacji wspomnianych wyżej mechanizmów zapalnych wykazano również zahamowanie proliferacji komórek, gromadzenie się mikroplastiku w ich wnętrzu oraz spadek ekspresji genów kodujących enzymy antyoksydacyjne, co zmniejszało zdolność komórek do neutralizowania wolnych rodników i nasilało efekt cytotoksyczny.
Podsumowanie:
Codzienna ekspozycja na mikroplastiki wymaga rzetelnej oceny zagrożenia poprzez interdyscyplinarne badania oparte na realistycznych stężeniach środowiskowych, uwzględniające długoterminowe skutki, właściwości fizykochemiczne cząstek oraz ich oddziaływania z innymi substancjami.
Introduction and objective:
In 2021, global plastic production reached 390.7 million tons and continues to increase annually. The accumulation of microplastic (MP) particles has been observed in all tissues and body fluids, with the respiratory tract, gastrointestinal tract and urinary system being particularly vulnerable to its toxic effects through direct. contact.
Review methods:
The PubMed database was searched using various combinations of specific key words: ‘microplastics’, ‘nanoplastics’, ‘lung diseases’, ‘intestinal diseases’, ‘renal diseases’, and ‘hepatic diseases’.
Brief description of the state of knowledge:
In response to microplastic stimulation, disturbances in oxidative stress balance and increased free radical formation have been observed in lung parenchyma, along with inflammation development via activation of the NF-κB pathway dependent on p38 phosphorylation and the Wnt/β-catenin pathway. Similar changes were observed in the gastrointestinal tract where microplastic-induced activation of the ROS–NF-κB/NLRP3/IL-1β/MLCK stress pathway led to damage to the intestinal barrier, alterations in gut microbiota composition, and disruptions in microbial metabolism. In the kidney parenchyma, in addition to the activation of the prior-mentioned inflammatory mechanisms, microplastic exposure resulted in inhibited cell proliferation, intracellular accumulation of microplastics, and a decrease in the expression of genes encoding antioxidant enzymes. This reduced the cells ability to neutralize free radicals and intensified cytotoxic effects.
Summary:
Understanding the health risks of daily microplastic exposure requires interdisciplinary studies that reflect realworld concentrations, emphasizing chronic effects, particle characteristics and their interactions with associated compounds.
In 2021, global plastic production reached 390.7 million tons and continues to increase annually. The accumulation of microplastic (MP) particles has been observed in all tissues and body fluids, with the respiratory tract, gastrointestinal tract and urinary system being particularly vulnerable to its toxic effects through direct. contact.
Review methods:
The PubMed database was searched using various combinations of specific key words: ‘microplastics’, ‘nanoplastics’, ‘lung diseases’, ‘intestinal diseases’, ‘renal diseases’, and ‘hepatic diseases’.
Brief description of the state of knowledge:
In response to microplastic stimulation, disturbances in oxidative stress balance and increased free radical formation have been observed in lung parenchyma, along with inflammation development via activation of the NF-κB pathway dependent on p38 phosphorylation and the Wnt/β-catenin pathway. Similar changes were observed in the gastrointestinal tract where microplastic-induced activation of the ROS–NF-κB/NLRP3/IL-1β/MLCK stress pathway led to damage to the intestinal barrier, alterations in gut microbiota composition, and disruptions in microbial metabolism. In the kidney parenchyma, in addition to the activation of the prior-mentioned inflammatory mechanisms, microplastic exposure resulted in inhibited cell proliferation, intracellular accumulation of microplastics, and a decrease in the expression of genes encoding antioxidant enzymes. This reduced the cells ability to neutralize free radicals and intensified cytotoxic effects.
Summary:
Understanding the health risks of daily microplastic exposure requires interdisciplinary studies that reflect realworld concentrations, emphasizing chronic effects, particle characteristics and their interactions with associated compounds.
Domagała M, Wiewióra J, Domańska I, Sagan A, Piśkiewicz M, Duda W, Majewska E. A comprehensive review of the impact of microplastics
on the Respiratory, Digestive and Renal Systems – mechanisms of toxicity and health implications. Med Og Nauk Zdr. 2025;31(3):149–155.
doi:10.26444/monz/208119
REFERENCJE (39)
1.
Gouin T, Boobis A, Cassee FR, Koelmans A, Price SC, Wagener S, Wright S. Dietary and inhalation exposure to nano- and microplastic particles and potential implications for human health. World Health Organization (WHO); 2022. doi:10.13140/RG.2.2.27459.07200.
2.
Adediran GA, Cox R, Jürgens MD, Morel E, Cross R, Carter H, Pereira MG, Read DS, Johnson AC. Fate and behaviour of microplastics (>25 μm) within the water distribution network, from water treatment works to service reservoirs and customer taps. Water Res. 2024;255:121508. doi:10.1016/j.watres.2024.121508.
3.
Borriello L, Scivicco M, Cacciola NA, Esposito F, Severino L, Cirillo T. Microplastics, a Global Issue: Human Exposure through Environmental and Dietary Sources. Foods. 2023 Sep 11;12(18):3396. doi:10.3390/foods12183396.
4.
Thompson RC, Courtene-Jones W, Boucher J, Pahl S, Raubenheimer K, Koelmans AA. Twenty years of microplastic pollution research – what have we learned? Science. 2024 Oct 25;386(6720):eadl2746. doi:10.1126/science.adl2746.
5.
Jamieson AJ, Brooks LSR, Reid WDK, Piertney SB, Narayanaswamy BE, Linley TD. Microplastics and synthetic particles ingested by deep-sea amphipods in six of the deepest marine ecosystems on Earth. R Soc Open Sci. 2019 Feb 27;6(2):180667. doi:10.1098/rsos.180667.
6.
González-Pleiter M, Edo C, Velázquez D, Casero-Chamorro MC, Leganés F, Quesada A, Fernández-Piñas F, Rosal R. First detection of microplastics in the freshwater of an Antarctic Specially Protected Area. Mar Pollut Bull. 2020 Dec;161(Pt B):111811. doi:10.1016/j.marpolbul.2020.111811.
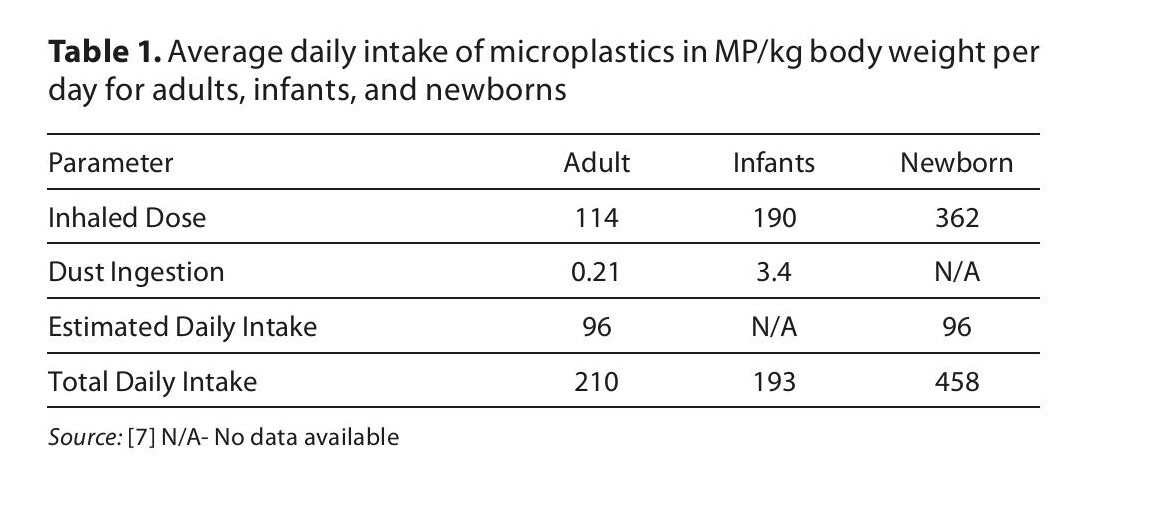
7.
Zuri G, Karanasiou A, Lacorte S. Microplastics: Human exposure assessment through air, water, and food. Environ Int. 2023 Sep;179:108150. doi:10.1016/j.envint.2023.108150. Epub 2023 Aug 14. PMID: 37607425.
8.
Zhu L, Kang Y, Ma M, Wu Z, Zhang L, Hu R, Xu Q, Zhu J, Gu X, An L. Tissue accumulation of microplastics and potential health risks in human. Sci Total Environ. 2024 Mar 10;915:170004. doi:10.1016/j.scitotenv.2024.170004.
9.
Zhu L, Zhu J, Zuo R, Xu Q, Qian Y, An L. Identification of microplastics in human placenta using laser direct infrared spectroscopy. Sci Total Environ. 2023 Jan 15;856(Pt 1):159060. doi:10.1016/j.scitotenv.2022.159060.
10.
Gou Z, Wu H, Li S, Liu Z, Zhang Y. Airborne micro- and nanoplastics: emerging causes of respiratory diseases. Part Fibre Toxicol. 2024 Dec 4;21(1):50. doi:10.1186/s12989-024-00613-6.
11.
Vasse GF, Melgert BN. Microplastic and plastic pollution: impact on respiratory disease and health. Eur Respir Rev. 2024 Jun 12;33(172):230226. doi:10.1183/16000617.0226-2023.
12.
Bengalli R, Zerboni A, Bonfanti P, Saibene M, Mehn D, Cella C, Ponti J, La Spina R, Mantecca P. Characterization of microparticles derived from waste plastics and their bio-interaction with human lung A549 cells. J Appl Toxicol. 2022 Dec;42(12):2030–2044. doi:10.1002/jat.4372.
13.
Woo JH, Seo HJ, Lee JY, Lee I, Jeon K, Kim B, Lee K. Polypropylene nanoplastic exposure leads to lung inflammation through p38-mediated NF-κB pathway due to mitochondrial damage. Part Fibre Toxicol. 2023 Jan 10;20(1):2. doi:10.1186/s12989-022-00512-8.
14.
Wu Q, Liu C, Liu D, Wang Y, Qi H, Liu X, Zhang Y, Chen H, Zeng Y, Li J. Polystyrene nanoplastics-induced lung apoptosis and ferroptosis via ROS-dependent endoplasmic reticulum stress. Sci Total Environ. 2024 Feb 20;912:169260. doi:10.1016/j.scitotenv.2023.169260.
15.
Lin S, Zhang H, Wang C, Su XL, Song Y, Wu P, Yang Z, Wong MH, Cai Z, Zheng C. Metabolomics Reveal Nanoplastic-Induced Mitochondrial Damage in Human Liver and Lung Cells. Environ Sci Technol. 2022 Sep 6;56(17):12483–12493. doi:10.1021/acs.est.2c03980.
16.
Tomonaga T, Higashi H, Izumi H, Nishida C, Sato K, Nakamura Y, Morimoto T, Higashi Y, Kojima T, Sakurai K, Yatera K, Morimoto Y. Comparison of lung disorders following intratracheal instillation of polystyrene microplastics with different surface functional groups. J Occup Health. 2025 Jan 7;67(1):uiaf006. doi:10.1093/joccuh/uiaf006.
17.
Li X, Zhang T, Lv W, Wang H, Chen H, Xu Q, Cai H, Dai J. Intratracheal administration of polystyrene microplastics induces pulmonary fibrosis by activating oxidative stress and Wnt/β-catenin signaling pathway in mice. Ecotoxicol Environ Saf. 2022 Mar 1;232:113238. doi:10.1016/j.ecoenv.2022.113238.
18.
Sun Z, Yang Z, Wang M, Huang C, Ren Y, Zhang W, Gao F, Cao L, Li L, Nie S. Paraquat induces pulmonary fibrosis through Wnt/β-catenin signaling pathway and myofibroblast differentiation. Toxicol Lett. 2020 Oct 15;333:170–183. doi:10.1016/j.toxlet.2020.08.004.
19.
Yang S, Zhang T, Ge Y, Cheng Y, Yin L, Pu Y, Chen Z, Liang G. Sentinel supervised lung-on-a-chip: A new environmental toxicology platform for nanoplastic-induced lung injury. J Hazard Mater. 2023 Sep 15;458:131962. doi:10.1016/j.jhazmat.2023.131962.
20.
Dong CD, Chen CW, Chen YC, Chen HH, Lee JS, Lin CH. Polystyrene microplastic particles: In vitro pulmonary toxicity assessment. J Hazard Mater. 2020 Mar 5;385:121575. doi:10.1016/j.jhazmat.2019.121575. Epub 2019 Nov 3. PMID: 31727530.
21.
Han Q, Gao X, Wang S, Wei Z, Wang Y, Xu K, Chen M. Co-exposure to polystyrene microplastics and di-(2-ethylhexyl) phthalate aggravates allergic asthma through the TRPA1-p38 MAPK pathway. Toxicol Lett. 2023 Aug 1;384:73–85. doi:10.1016/j.toxlet.2023.07.013.
22.
Chen C, Liu F, Quan S, Chen L, Shen A, Jiao A, Qi H, Yu G. Microplastics in the Bronchoalveolar Lavage Fluid of Chinese Children: Associations with Age, City Development, and Disease Features. Environ Sci Technol. 2023 Aug 29;57(34):12594–12601. doi:10.1021/acs.est.3c0177.
23.
Osman AI, Hosny M, Eltaweil AS, Omar S, Elgarahy AM, Farghali M, Yap PS, Wu YS, Nagandran S, Batumalaie K, Gopinath SCB, John OD, Sekar M, Saikia T, Karunanithi P, Hatta MHM, Akinyede KA. Microplastic sources, formation, toxicity and remediation: a review. Environ Chem Lett. 2023 Apr 4:1–41. doi: 10.1007/s10311-023-01593-3.
24.
Yan Z, Liu Y, Zhang T, Zhang F, Ren H, Zhang Y. Analysis of Microplastics in Human Feces Reveals a Correlation between Fecal Microplastics and Inflammatory Bowel Disease Status. Environ Sci Technol. 2022 Jan 4;56(1):414–421. doi:10.1021/acs.est.1c03924.
25.
Zeng G, Li J, Wang Y, Su J, Lu Z, Zhang F, Ding W. Polystyrene microplastic-induced oxidative stress triggers intestinal barrier dysfunction via the NF-κB/NLRP3/IL-1β/MCLK pathway. Environ Pollut. 2024 Mar 15;345:123473. doi:10.1016/j.envpol.2024.123473.
26.
Yao FC, Jin CX, Liang H, Zhang Y, Gu Y, Song FB, Zhou Z, Sun JL, Luo J. Microplastics weaken the digestion and absorption functions in the golden pompano (Trachinotus blochii) by affecting the intestinal structure, bacteria and metabolites. Chemosphere. 2024 Aug;362:142415. doi:10.1016/j.chemosphere.2024.142415.
27.
Souza-Silva TG, Oliveira IA, Silva GGD, Giusti FCV, Novaes RD, Paula HAA. Impact of microplastics on the intestinal microbiota: A systematic review of preclinical evidence. Life Sci. 2022 Apr 1;294:120366. doi:10.1016/j.lfs.2022.120366.
28.
Zhang X, Wang H, Peng S, Kang J, Xie Z, Tang R, Xing Y, He Y, Yuan H, Xie C, Liu Y. Effect of microplastics on nasal and intestinal microbiota of the high-exposure population. Front Public Health. 2022 Oct 28;10:1005535. doi:10.3389/fpubh.2022.1005535.
29.
Zhang Y, Yuan J, Mao T. Impact of microplastics exposure on liver health: A comprehensive meta-analysis. Comp Biochem Physiol C Toxicol Pharmacol. 2025 Feb;288:110080. doi:10.1016/j.cbpc.2024.110080.
30.
Zhang H, Gao Y, Zheng Y, Zheng J, He J, Shi J, Zhang K, Song Y, Zhang J, Shi X, Zhang R, Ding Y, Jing Y, Xu K, Wang J. Potential toxicity of microplastics on vertebrate liver: A systematic review and meta-analysis. Ecotoxicol Environ Saf. 2024 Nov 1;286:117166. doi:10.1016/j.ecoenv.2024.117166.
31.
Shi Y, Hong R, Fan Z, Huan R, Gao Y, Ma M, Liu T, Pan C. Chronic environmental exposure to polystyrene microplastics increases the risk of nonalcoholic fatty liver disease. Toxicology. 2025 Feb;511:154067. doi:10.1016/j.tox.2025.154067.
32.
Wang Q, Wu Y, Zhang W, Shen T, Li H, Wu J, Zhang L, Qin L, Chen R, Gu W, Sun Q, Liu C, Li R. Lipidomics and transcriptomics insight into impacts of microplastics exposure on hepatic lipid metabolism in mice. Chemosphere. 2022 Dec;308(Pt 3):136591. doi:10.1016/j.chemosphere.2022.136591.
33.
Horvatits T, Tamminga M, Liu B, Sebode M, Carambia A, Fischer L, Püschel K, Huber S, Fischer EK. Microplastics detected in cirrhotic liver tissue. EBioMedicine. 2022 Aug;82:104147. doi:10.1016/j.ebiom.2022.104147.
34.
Zhang D, Wu C, Liu Y, Li W, Li S, Peng L, Kang L, Ullah S, Gong Z, Li Z, Ding D, Jin Z, Huang H. Microplastics are detected in human gallstones and have the ability to form large cholesterol-microplastic heteroaggregates. J Hazard Mater. 2024 Apr 5;467:133631. doi:10.1016/j.jhazmat.2024.133631.
35.
Xu M, Niu H, Wu L, Xing M, Mo Z, Chen Z, Li X, Lou X. Impact of Microplastic Exposure on Blood Glucose Levels and Gut Microbiota: Differential Effects under Normal or High-Fat Diet Conditions. Metabolites. 2024 Sep 18;14(9):504. doi:10.3390/metabo14090504.
36.
Huang H, Lei P, Yu H, Du J, Wu B, Wang H, Yang Q, Cheng Y, Sun D, Wan L. Micro/nano plastics in the urinary system: Pathways, mechanisms, and health risks. Environ Int. 2024 Nov;193:109109. doi:10.1016/j.envint.2024.109109.
37.
Goodman KE, Hua T, Sang Q-XA. Effects of Polystyrene Microplastics on Human Kidney and Liver Cell Morphology, Cellular Proliferation, and Metabolism. ACS Omega. 2022 Sep 19;7(38):34136–53.
38.
Meng X, Yin K, Zhang Y, Wang D, Lu H, Hou L, Zhao H, Xing M. Polystyrene microplastics induced oxidative stress, inflammation and necroptosis via NF-κB and RIP1/RIP3/MLKL pathway in chicken kidney. Toxicology. 2022 Aug;478:153296. doi:10.1016/j.tox.2022.153296.
39.
Wang YL, Lee YH, Hsu YH, Chiu IJ, Huang CC, Huang CC, Chia ZC, Lee CP, Lin YF, Chiu HW. The Kidney-Related Effects of Polystyrene Microplastics on Human Kidney Proximal Tubular Epithelial Cells HK-2 and Male C57BL/6 Mice. Environ Health Perspect. 2021 May;129(5):57003. doi:10.1289/EHP7612.
Przetwarzamy dane osobowe zbierane podczas odwiedzania serwisu. Realizacja funkcji pozyskiwania informacji o użytkownikach i ich zachowaniu odbywa się poprzez dobrowolnie wprowadzone w formularzach informacje oraz zapisywanie w urządzeniach końcowych plików cookies (tzw. ciasteczka). Dane, w tym pliki cookies, wykorzystywane są w celu realizacji usług, zapewnienia wygodnego korzystania ze strony oraz w celu monitorowania ruchu zgodnie z Polityką prywatności. Dane są także zbierane i przetwarzane przez narzędzie Google Analytics (więcej).
Możesz zmienić ustawienia cookies w swojej przeglądarce. Ograniczenie stosowania plików cookies w konfiguracji przeglądarki może wpłynąć na niektóre funkcjonalności dostępne na stronie.
Możesz zmienić ustawienia cookies w swojej przeglądarce. Ograniczenie stosowania plików cookies w konfiguracji przeglądarki może wpłynąć na niektóre funkcjonalności dostępne na stronie.