Online first
Bieżący numer
Archiwum
O czasopiśmie
Polityka etyki publikacyjnej
System antyplagiatowy
Instrukcje dla Autorów
Instrukcje dla Recenzentów
Rada Redakcyjna
Komitet Redakcyjny
Recenzenci
Wszyscy recenzenci
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
Kontakt
Bazy indeksacyjne
Klauzula przetwarzania danych osobowych (RODO)
PRACA ORYGINALNA
Wpływ depresji na jakość życia osób w wieku podeszłym – badania pilotażowe
1
Department of Gerontology, Department of Public Health, Faculty of Health Sciences, Medical University, Wrocław, Poland
2
Mental Health Centre, LUX MED / PROFEMED Group, Warsaw, Poland
3
Ombudsman for Patients’ Rights, Warsaw, Poland
4
Chair of Civil Law, University of Warsaw, Poland
5
Higher School of Rehabilitation, Warsaw, Poland
Med Og Nauk Zdr. 2021;27(2):199-204
SŁOWA KLUCZOWE
DZIEDZINY
STRESZCZENIE
Wprowadzenie i cel:
Depresja jest jedną z najczęstszych chorób u osób starszych. Dotyka ok. 15–20% osób w wie-ku powyżej 65 lat. Objawia się przede wszystkim obniżeniem nastroju, sprawności intelektualnej, koncentracji i samooceny, anhedonią, zmianą apetytu, zaburzeniami snu oraz uczuciem zmęczenia i utratą energii. W niniejszym artykule autorzy ocenią wpływ depresji na jakość życia osób starszych.
Materiał i metody:
W anonimowym badaniu wzięło udział 140 (100%) hospitalizowanych pacjentów oddziału geriatrycznego, z których większość (73,57%) stanowiły kobiety. Respondenci byli w wieku 65–88 lat, przy czym największa grupa (54,29%) mieściła się w przedziale wiekowym 76–85 lat.
Wyniki:
Łagodną depresję stwierdzono u 37,86%, a ciężką u 12,14% badanych. Większość seniorów (42,14%) oceniła swoją jakość życia jako dobrą. Ponad połowa badanych (55,71%) deklarowała pewność siebie, 45,00% rzadko doświadczało obniżenia nastroju, rozpaczy, lęku lub obniżonego nastroju, 40,00% nie było zadowolonych ze swojego stanu zdrowia, 37,14% nie było zadowolonych z jakości snu, u 22,14% ból znacząco wpływał na codzienne życie. Pacjenci z depresją gorzej oceniali swoją jakość życia w sferach: somatycznej, psychicznej, społecznej i środowiskowej (p < 0,001). Stwierdzono istotne statystycznie zależności między oceną jakości życia w dziedzinie somatycznej a stanem zdrowia seniorów (p < 0,05) oraz między oceną jakości życia w dziedzinie środowiskowej a liczbą chorób (p = 0,034)
Wnioski:
Pacjenci z depresją oceniają swoją jakość życia gorzej we wszystkich aspektach. U osób starszych jakość życia zależy od stanu zdrowia i liczby zdiagnozowanych chorób. Seniorzy mieszkający z rodziną lepiej oceniają swoją jakość życia.
Depresja jest jedną z najczęstszych chorób u osób starszych. Dotyka ok. 15–20% osób w wie-ku powyżej 65 lat. Objawia się przede wszystkim obniżeniem nastroju, sprawności intelektualnej, koncentracji i samooceny, anhedonią, zmianą apetytu, zaburzeniami snu oraz uczuciem zmęczenia i utratą energii. W niniejszym artykule autorzy ocenią wpływ depresji na jakość życia osób starszych.
Materiał i metody:
W anonimowym badaniu wzięło udział 140 (100%) hospitalizowanych pacjentów oddziału geriatrycznego, z których większość (73,57%) stanowiły kobiety. Respondenci byli w wieku 65–88 lat, przy czym największa grupa (54,29%) mieściła się w przedziale wiekowym 76–85 lat.
Wyniki:
Łagodną depresję stwierdzono u 37,86%, a ciężką u 12,14% badanych. Większość seniorów (42,14%) oceniła swoją jakość życia jako dobrą. Ponad połowa badanych (55,71%) deklarowała pewność siebie, 45,00% rzadko doświadczało obniżenia nastroju, rozpaczy, lęku lub obniżonego nastroju, 40,00% nie było zadowolonych ze swojego stanu zdrowia, 37,14% nie było zadowolonych z jakości snu, u 22,14% ból znacząco wpływał na codzienne życie. Pacjenci z depresją gorzej oceniali swoją jakość życia w sferach: somatycznej, psychicznej, społecznej i środowiskowej (p < 0,001). Stwierdzono istotne statystycznie zależności między oceną jakości życia w dziedzinie somatycznej a stanem zdrowia seniorów (p < 0,05) oraz między oceną jakości życia w dziedzinie środowiskowej a liczbą chorób (p = 0,034)
Wnioski:
Pacjenci z depresją oceniają swoją jakość życia gorzej we wszystkich aspektach. U osób starszych jakość życia zależy od stanu zdrowia i liczby zdiagnozowanych chorób. Seniorzy mieszkający z rodziną lepiej oceniają swoją jakość życia.
Introduction and objective:
Depression is among the most common diseases in the elderly. It affects ca. 15–20% of people aged over 65 years. The symptomatology of depression is manifested mainly by decreased mood, intellectual skills, concentration and self-esteem, anhedonia, change in appetite, sleep disorders, and the feeling of fatigue and loss of energy. The aim of the article is to assess the impact of depression on the quality of life in elderly people.
Material and methods:
The anonymous study involved 140 (100%) hospitalized patients of a geriatric ward, most of whom (73.57%) were women. The respondents were 65–88 years old, with the largest group (54.29%) in the age range 76–85 years
Results:
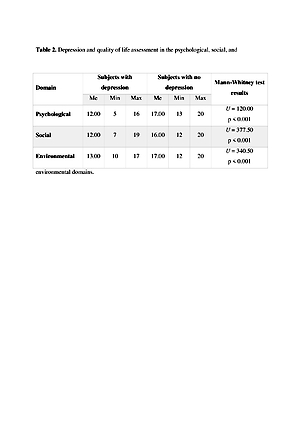
Mild depression was found in 37.86%, and severe depression in 12.14% of the respondents. Most seniors (42.14%) assessed their quality of life as good. More than half of the subjects (55.71%) declared self-assurance, 45.00% rarely experienced low spirits, despair, fear, or decreased mood, 40.00% were not satisfied with their health, 37.14% were not satisfied with their sleep quality, in 22.14% pain significantly influenced their everyday life. Patients with depression indicated worse assessments of their quality of life in the somatic, psychological, social, and environmental domains (p < 0.001). Statistically significant relationships were observed between quality of life assessment in the somatic domain and the seniors’ health status (p < 0.05), as well as between quality of life assessment in the environmental domain and the number of diseases (p = 0.034
Conclusions:
Patients with depression scored their quality of life worse in all domains. In elderly people, quality of life depends on their health status and the number of diagnosed diseases. Seniors living with families indicated better assessments of their quality of life.
Depression is among the most common diseases in the elderly. It affects ca. 15–20% of people aged over 65 years. The symptomatology of depression is manifested mainly by decreased mood, intellectual skills, concentration and self-esteem, anhedonia, change in appetite, sleep disorders, and the feeling of fatigue and loss of energy. The aim of the article is to assess the impact of depression on the quality of life in elderly people.
Material and methods:
The anonymous study involved 140 (100%) hospitalized patients of a geriatric ward, most of whom (73.57%) were women. The respondents were 65–88 years old, with the largest group (54.29%) in the age range 76–85 years
Results:
Mild depression was found in 37.86%, and severe depression in 12.14% of the respondents. Most seniors (42.14%) assessed their quality of life as good. More than half of the subjects (55.71%) declared self-assurance, 45.00% rarely experienced low spirits, despair, fear, or decreased mood, 40.00% were not satisfied with their health, 37.14% were not satisfied with their sleep quality, in 22.14% pain significantly influenced their everyday life. Patients with depression indicated worse assessments of their quality of life in the somatic, psychological, social, and environmental domains (p < 0.001). Statistically significant relationships were observed between quality of life assessment in the somatic domain and the seniors’ health status (p < 0.05), as well as between quality of life assessment in the environmental domain and the number of diseases (p = 0.034
Conclusions:
Patients with depression scored their quality of life worse in all domains. In elderly people, quality of life depends on their health status and the number of diagnosed diseases. Seniors living with families indicated better assessments of their quality of life.
Wróblewska I, Bartyzel M, Chmielowiec B, Puścion M, Chmielewski JP. The impact of depression on the quality of life in elderly people. Med Og Nauk Zdr. 2021; 27(2): 199–204. doi: 10.26444/monz/136243
REFERENCJE (35)
1.
Dols A, Kupka RW, van Lammeren A, et al. The prevalence of late-life mania: a review. Bipolar Disord. 2014; 16(2): 113–118. https://doi.org /10.1111/ bd i.12104.
2.
Sajatovic M, Strejilevich SA, Gildengers AG, et al. A report on older-age bipolar disorder from the International Society for Bipolar Disorders Task Force. Bipolar Disord. 2015; 17(7): 689–704. https://doi.org/10.1111/bd i.12331.
3.
Aziz R, Steffens D. Overlay of Late-Life Depression and Cognitive Impairment. Focus. 2017; 15(1): 35–41. https://doi.org/10.1176/appi.f....
4.
Livingston G, Huntley J, Sommerlad A, et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet. 2020 https://doi.org/10.1016/s0140-....
5.
Orgeta V, Mukadam N, Sommerlad A, et al. The Lancet Commission on Dementia Prevention, Intervention, and Care: A call for action. Ir J Psychol Med. 2018; 36(2): 85–88. https://doi.org/10.1017/ipm.20....
6.
Kivimäki M, Singh-Manoux A. Prevention of dementia by targeting risk factors. Lancet. 2018; 391(10130): 1574–1575. https://doi.org/10.1016/s0140-....
7.
Tipton PW, Graff-Radford NR. Prevention of late-life dementia what works and what does not. Pol Arch Intern Med. 2018; 128: 310–316. https://doi.org/10.20452/pamw.....
8.
Singh-Manoux A, Dugravot A, Fournier A, et al. Trajectories of Depressive Symptoms Before Diagnosis of Dementia: A 28-Year Follow-up Study. JAMA Psychiatry. 2017; 74(7): 712–718. https://doi.org/10.1001/jamaps... y.2017.0660.
9.
Imaoka M, Nakao H, Nakamura M, et al. Associations between depressive symptoms and geriatric syndromes in community-dwelling older adults in Japan: A cross-sectional study. Prev Med Rep. 2021; (10)22: 101353. https://doi.org/10.1016/j.pmed....
10.
Warren JD, Bamiou DE. Prevention of dementia by targeting risk factors. Lancet. 2018; 391(10130): 1575. https://doi.org/10.1016/S0140-... 0579 - 8.
11.
Humańska MA, Kędzierska-Kornatowska K. Correlation among intensification of depressive states and the feeling of life quality in the elderly. Psychogeriatria Polska. 2009; 6(1): 15–22. http://www.fozp.org.pl/wpconte....
12.
Pilania M, Yadav V, Bairwa M, et al. Prevalence of depression among the elderly (60 years and above) population in India, 1997–2016: a systematic review and meta-analysis. BMC Public Health. 2019; 19(1): 832. https://doi.org/10.1186/s12889....
13.
Hanyu H. Prevention of Dementia-with Special Reference to Lifestyle and Vascular Risk Factors. Brain Nerve. 2018; 70(3): 191–198. https://doi.org /10.11477/m f.141620 0981.
14.
Park JS, Lee J, Jung ES, et al. Brain somatic mutations observed in Alzheimer’s disease associated with aging and dysregulation of tau phosphorylation. Nature Communications. 2019; 10(1): 3090. https://doi.org/10.1038/s41467....
15.
Sandberg M, Ahlström G, Axmon A. et al. Somatic healthcare utilisation patterns among older people with intellectual disability: an 11-year register study. BMC Health Serv Res. 2016; 16: 642 https://doi.org/10.1186/s12913....
16.
Kessler RC, Bromet EJ. The Epidemiology of Depression Across Cultures. Annu Rev Public Health. 2013; 34(1): 119–138. https://doi.org/10.1146/annure....
17.
Dixon J, Karagiannidou M, Knapp M. The Effectiveness of Advance Care Planning in Improving End-of-Life Outcomes for People With Dementia and Their Carers: A Systematic Review and Critical Discussion. J Pain Symptom Manage. 2018; 55(1): 132–150.e1. https://doi.org/10.1016/j.jpai....
18.
Tunvirachaisakul C, Gould RL, Coulson MC, et al. Predictors of treatment outcome in depression in later life: A systematic review and meta-analysis. J Affect Disord. 2018; 227: 164–182. https://doi.org/10.1016/j.jad.....
19.
Andre KKA, McKibbin CL, Wykes TL, et al. Depression Treatment Among Rural Older Adults: Preferences and Factors Influencing Future Service Use. Clin Gerontol. 2013; 36(3): 241–259. https://doi.org/10.1080/073171....
20.
Burzynska M, Bryla M, Bryla P, et al. Factors determining the use of social support services among elderly people living in a city environment in Poland. Health Soc Care Community. 2015; 24(6): 758–768. https://doi.org /10.1111/hsc.12259.
21.
Kolotkin RL, Binks M, Crosby RD, et al. Obesity and sexual Quality of Life. Obesity. 2006; 14(3): 472–479. https://doi.org/10.1038/oby.20....
22.
Maciejasz M, Łątkowski W, Timoszuk S. et al. Selected aspects of quality of life of people aged 60+ in Poland in qualitative research, Studia Ekonomiczne. 2015; 223: 257–267. http://yadda.icm.edu.pl/yadda/....
23.
Huber D, Milne S, Hyde KF. Constraints and facilitators for senior tourism. Tourism Management Perspectives, 2018; 27: 55–67. https://doi.org/10.1016/j.tmp.....
24.
Beard JR, de Carvalho IA, Sumi Y, et al. Healthy ageing: moving forward. Bull World Health Organ. 2017; 95(11): 730–730A. https://doi.org/10.2471/BLT.17....
25.
Chatterji S, Byles J, Cutler D, et al. Health, functioning, and disability in older adults–present status and future implications. Lancet. 2015; 385(9967): 563–75. https://doi.org/10.1016/S0140-....
26.
Su D, Wu XN, Zhang YX, et al. Depression and social support between China’ rural and urban empty-nest elderly. Arch Gerontol Geriatr. 2012; 55(3): 564–569. https://doi.org/10.1016/j.arch....
27.
Ornstein KA, Kelley AS, Bollens-Lund E, et al. A National Profile Of End-Of-Life Caregiving In The United States. Health Aff. 2017; 36(7): 1184–1192. https://doi.org/10.1377/hlthaf....
28.
Moyle W, Murfield J, Venturto L, et al.Dementia and its influence on quality of life and what it means to be valued: Family members’ perceptions. Dementia. 2013; 13(3): 412–425. https://doi.org/10.1177/147130....
29.
Na L, Streim JE. Psychosocial Well-Being Associated With Activity of Daily Living Stages Among Community-Dwelling Older Adults. Gerontol Geriatr Med. 2017; 3: 233372141770001. https://doi.org/10.1177/233372....
30.
Starczewska ME, Prociak L, Rybicka A. Assessment of the functionalcapacity and the risk of depression among seniors. Pielęg Pol. 2019; 3(73): 258–264. https://doi.org/10.20883/pielp....
31.
Knyszyńska A, Radecka A, Bryczkowska I. et al. The relationship between functional efficiency and the level of depression among residents of Social Welfare Houses. Gerontol Pol. 2019; 27: 144–149. https://www.akademiamedycyny.p....
32.
Ostrzyżek A, Marcinkowski J. Dimensions of the quality of life in old age. Probl Hig Epidemiol. 2009; 90(4): 465–469. http://www.phie.pl/pdf/phe-200....
33.
Vogelzangs N, Kritchevsky S, Beekman A. Depressive symptoms and change in abdominal obesity in older persons, Arch Gen Psychiatry. 2008; 65(12): 1386–1393. https://doi.org/10.1001/archps....
34.
Pacian A, Kulik T, Chruściel P, et al. Quality of life and risk of depression among elderly people. Hygeia Public Health. 2014; 49(4): 820- 824. http://www.h-ph.pl/pdf/hyg-201....
35.
Fernandez-Munoz JJ, Ciqaran-Mendez M, Navarro-Pardo E, et al. Is the association between health-related quality of life and fatigue mediated by depression in patients with multiple sclerosis? A Spanish cross-sectional study. BMJ Open. 2018; 8(1): e016297. https://doi.org/10.1136/bmjope....
Udostępnij
ARTYKUŁ POWIĄZANY
Przetwarzamy dane osobowe zbierane podczas odwiedzania serwisu. Realizacja funkcji pozyskiwania informacji o użytkownikach i ich zachowaniu odbywa się poprzez dobrowolnie wprowadzone w formularzach informacje oraz zapisywanie w urządzeniach końcowych plików cookies (tzw. ciasteczka). Dane, w tym pliki cookies, wykorzystywane są w celu realizacji usług, zapewnienia wygodnego korzystania ze strony oraz w celu monitorowania ruchu zgodnie z Polityką prywatności. Dane są także zbierane i przetwarzane przez narzędzie Google Analytics (więcej).
Możesz zmienić ustawienia cookies w swojej przeglądarce. Ograniczenie stosowania plików cookies w konfiguracji przeglądarki może wpłynąć na niektóre funkcjonalności dostępne na stronie.
Możesz zmienić ustawienia cookies w swojej przeglądarce. Ograniczenie stosowania plików cookies w konfiguracji przeglądarki może wpłynąć na niektóre funkcjonalności dostępne na stronie.