RESEARCH PAPER
Antibiotics use, urgency and beliefs about antibiotics in the case of acute pharyngitis
1
Wojewódzki Szpital Specjalistyczny im. Stefana Kardynała Wyszyńskiego, Polska
2
Samodzielny Publiczny Szpital Kliniczny Nr 4 w Lublinie, Polska
3
Lubelska Akademia WSEI, Polska
Corresponding author
Mikołaj Porzak
WOJEWÓDZKI SZPITAL SPECJALISTYCZNY im. Stefana Kardynała Wyszyńskiego, Aleja Kraśnicka 100, 20-718, Lublin, Polska
WOJEWÓDZKI SZPITAL SPECJALISTYCZNY im. Stefana Kardynała Wyszyńskiego, Aleja Kraśnicka 100, 20-718, Lublin, Polska
Med Og Nauk Zdr. 2024;30(1):41-48
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
The study investigates patterns of antibiotic use among patients in the Lublin area of eastern Poland, aiming to understand the motivations behind self- -medication. Specifically, the study focuses on identifying repeatable patterns of antibiotic use and assessing differences in self-medication behaviours based on these patterns.
Material and methods:
A survey was conducted at a Family Doctor›s clinic in Lublin, involving primary care patients. Participants completed an anonymous questionnaire consisting of three sections: demographics and general health assessment, pharyngitis occurrence and management, and beliefs about antibiotic use, pain sensitivity, and urgency.
Results:
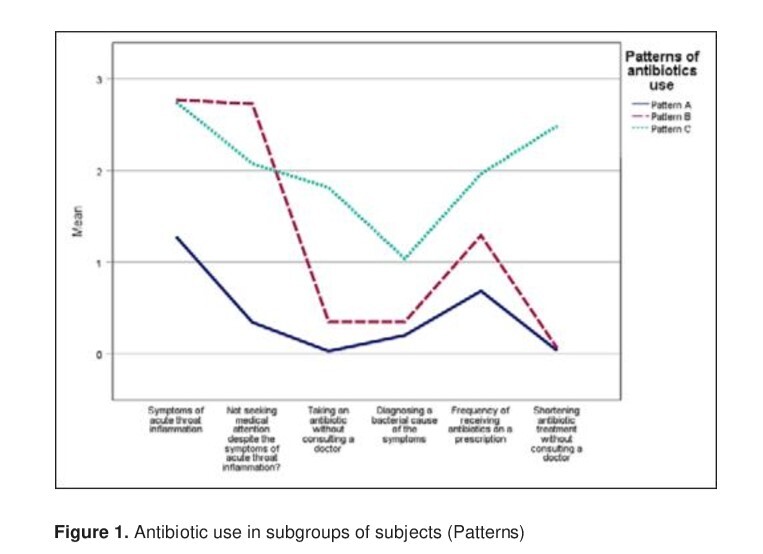
Three distinct subgroups emerged from the analysis: Pattern A (62%) – rarely suffered from acute pharyngitis and rarely used antibiotics without medical consultation or shortened the period of antibiotic treatment; Pattern B (29%) – often suffered from acute pharyngitis and rarely used antibiotics without medical consultation, or shortened the period of antibiotic treatment; Pattern C (9%) – Frequently self-medicated with antibiotics, often without medical consultation. These patterns correlated with subjective health assessment, pain sensitivity, urgency, and beliefs about antibiotics.
Conclusions:
The study highlights diverse attitudes towards acute pharyngitis symptoms and antibiotic use. Physician alertness should focus on patients with high urgency levels, severe pain, recurrent infections, prior antibiotic self-medication, and a propensity to shorten antibiotic therapy. Understanding these patterns is crucial for tailored interventions promoting rational antibiotic use. Further research should explore similar behaviour patterns in other infectious diseases to guide clinical decision-making and mitigate antibiotic resistance.
The study investigates patterns of antibiotic use among patients in the Lublin area of eastern Poland, aiming to understand the motivations behind self- -medication. Specifically, the study focuses on identifying repeatable patterns of antibiotic use and assessing differences in self-medication behaviours based on these patterns.
Material and methods:
A survey was conducted at a Family Doctor›s clinic in Lublin, involving primary care patients. Participants completed an anonymous questionnaire consisting of three sections: demographics and general health assessment, pharyngitis occurrence and management, and beliefs about antibiotic use, pain sensitivity, and urgency.
Results:
Three distinct subgroups emerged from the analysis: Pattern A (62%) – rarely suffered from acute pharyngitis and rarely used antibiotics without medical consultation or shortened the period of antibiotic treatment; Pattern B (29%) – often suffered from acute pharyngitis and rarely used antibiotics without medical consultation, or shortened the period of antibiotic treatment; Pattern C (9%) – Frequently self-medicated with antibiotics, often without medical consultation. These patterns correlated with subjective health assessment, pain sensitivity, urgency, and beliefs about antibiotics.
Conclusions:
The study highlights diverse attitudes towards acute pharyngitis symptoms and antibiotic use. Physician alertness should focus on patients with high urgency levels, severe pain, recurrent infections, prior antibiotic self-medication, and a propensity to shorten antibiotic therapy. Understanding these patterns is crucial for tailored interventions promoting rational antibiotic use. Further research should explore similar behaviour patterns in other infectious diseases to guide clinical decision-making and mitigate antibiotic resistance.
REFERENCES (30)
1.
Organization WH. Guidelines for the regulatory assessment of medicinal products for use in self-medication. 2000 [cited 9 Jan 2024]. Available: https://iris.who.int/handle/10....
2.
Montastruc J-L, Bondon-Guitton E, Abadie D, Lacroix I, Berreni A, Pugnet G, et al. Pharmacovigilance, risks and adverse effects of self-medication. Therapies. 2016;71:257–262. doi:10.1016/j.therap.2016.02.012.
3.
Ahmed I, King R, Akter S, Akter R, Aggarwal VR. Determinants of antibiotic self-medication: A systematic review and meta-analysis. Res Soc Adm Pharm RSAP. 2023;19:1007–1017. doi:10.1016/j.sapharm.2023.03.009.
4.
AZAMI-AGHDASH S, MOHSENI M, ETEMADI M, ROYANI S, MOOSAVI A, NAKHAEE M. Prevalence and Cause of Self-Medication in Iran: A Systematic Review and Meta-Analysis Article. Iran J Public Health. 2015;44:1580–1593.
5.
Sailler L, Pugnet G, Montastruc J-L. [Self-medication]. Rev Prat. 2012;62: 1463–1467.
6.
Lee CHJ, Norris P, Duck IM, Sibley CG. Demographic and Psychological Factors Associated with Feelings of Antibiotic Entitlement in New Zealand. Antibiotics. 2018;7:82. doi:10.3390/antibiotics7030082.
7.
Papachristou H, Nederkoorn C, Jansen A. Neuroticism and Negative Urgency in Problematic Alcohol Use: A Pilot Study. Subst Use Misuse. 2016;51:1529–1533.
8.
Teh WL, Liu J, Chandwani N, Lee YW, Tor P-C, Subramaniam M, et al. Emotional urgency predicts bipolar symptoms, severity, and suicide attempt better than non-emotional impulsivity: a cross-sectional study. Front Psychol. 2023;14:1277655. doi:10.3389/fpsyg.2023.1277655.
9.
Gonçalves SF, Izquierdo AM, Bates RA, Acharya A, Matto H, Sikdar S. Negative Urgency Linked to Craving and Substance Use Among Adults on Buprenorphine or Methadone. J Behav Health Serv Res. 2024;51: 114–122. doi:10.1007/s11414-023-09845-4.
10.
Luba R, Earleywine M, Farmer S, Slavin M, Mian M, Altman B. The Role of Impulsivity and Expectancies in Predicting Marijuana Use: An Application of the Acquired Preparedness Model. J Psychoactive Drugs. 2018;50:411–419.
11.
Karakonstantis S, Kalemaki D. Antimicrobial overuse and misuse in the community in Greece and link to antimicrobial resistance using methicillin-resistant S. aureus as an example. J Infect Public Health. 2019;12:460–464. doi:10.1016/j.jiph.2019.03.017.
12.
Antimicrobial resistance surveillance in Europe 2022–2020 data. 26 Jan 2022 [cited 23 Jan 2024]. Available: https://www.ecdc.europa.eu/en/....
13.
Antimicrobial resistance in the EU/EEA (EARS-Net) – Annual epidemiological report for 2022. 2022.
14.
Murray CJL, Ikuta KS, Sharara F, Swetschinski L, Aguilar GR, Gray A, et al. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. The Lancet. 2022;399:629–655. doi:10.1016/S0140-6736(21)02724-0.
15.
Drug-Resistant Infections: A Threat to Our Economic Future. In: World Bank [Internet]. [cited 29 Jan 2024]. Available: https://www.worldbank.org/en/t....
16.
Nugent SM, Lovejoy TI, Shull S, Dobscha SK, Morasco BJ. Associations of Pain Numeric Rating Scale Scores Collected during Usual Care with Research Administered Patient Reported Pain Outcomes. Pain Med. 2021;22: 2235–2241. doi:10.1093/pm/pnab110.
17.
Groskurth K, Nießen D, Rammstedt B, Lechner CM. The impulsive behavior short scale–8 (I-8): A comprehensive validation of the English-language adaptation. PLOS ONE. 2022;17: e0273801. doi:10.1371/journal.pone.0273801.
18.
Zhang Z, Yuan K-H. Robust Coefficients Alpha and Omega and Confidence Intervals With Outlying Observations and Missing Data. Educ Psychol Meas. 2016;76:387–411.
19.
Backhaus K, Erichson B, Gensler S, Weiber R, Weiber T. Cluster Analysis. Multivariate Analysis: An Application-Oriented Introduction. Wiesbaden: Springer Fachmedien Wiesbaden; 2023. pp. 453–532. doi 10.1007/978-3-658-40411-6_8.
20.
Greve KW, Bianchini KJ. Setting empirical cut-offs on psychometric indicators of negative response bias: a methodological commentary with recommendations. Arch Clin Neuropsychol. 2004;19:533–541. doi:10.1016/j.acn.2003.08.002.
21.
OECD. Embracing a One Health Framework to Fight Antimicrobial Resistance. OECD; 2023. doi:10.1787/ce44c755-en.
22.
Alanazi A, Almuhaya R, Almohaimeed M, Alahmari N, Abdulrahim N, Basyouni M, et al. Impact of Antibiotic De-Escalation on Antibiotic Consumption, Length of Hospitalization, Mortality, and Cost: A Systematic Review and Meta-Analysis. Pharmacoepidemiol 2813–0618. 2023;2:289–306.
23.
Thong ISK, Jensen MP, Miró J, Tan G. The validity of pain intensity measures: what do the NRS, VAS, VRS, and FPS-R measure? Scand J Pain. 2018;18: 99–107. doi:10.1515/sjpain-2018-0012.
24.
Clark CW, Yang JC, Tsui S-L, Ng K-F, Clark SB. Unidimensional pain rating scales: a multidimensional affect and pain survey (MAPS) analysis of what they really measure. Pain. 2002;98:241–247. doi:10.1016/ S0304-3959(01)00474-2.
25.
Keiko Yamada, Tomoko Fujii, Yasuhiko Kubota, Kenta Wakaizumi, Hiroyuki Oka, Ko Matsudaira. Negative effect of anger on chronic pain intensity is modified by multiple mood states other than anger: A large population-based cross-sectional study in Japan. Mod Rheumatol. 2022;32: 650–657.
26.
Willis BH, Coomar D, Baragilly M. Comparison of Centor and McIsaac scores in primary care: a meta-analysis over multiple thresholds. Br J Gen Pract. 2020;70: e245–e254. doi:10.3399/bjgp20X708833.
27.
Snow V, Mottur-Pilson C, Cooper RJ, Hoffman JR, American Academy of Family Physicians, American College of Physicians-American Society of Internal Medicine, et al. Principles of appropriate antibiotic use for acute pharyngitis in adults. Ann Intern Med. 2001;134:506–508. doi:10.7326/0003-4819-134-6-200103200-00018.
28.
Paź A, Arcimowicz M. Antibiotic Therapy for Acute Upper Respiratory Tract Infections and Middle Ear Infections in Adults. Pol Przegląd Otorynolaryngologiczny. 2018;7:1–7. doi:10.5604/01.3001.0011.6681.
29.
Linder JA, Chan JC, Bates DW. Evaluation and Treatment of Pharyngitis in Primary Care Practice: The Difference Between Guidelines Is Largely Academic. Arch Intern Med. 2006;166:1374–1379. doi:10.1001/ archinte.166.13.1374.
30.
Chen Q, Li D, Beiersmann C, Neuhann F, Moazen B, Lu G, et al. Risk factors for antibiotic resistance development in healthcare settings in China: a systematic review. Epidemiol Infect. 2021;149: e141. doi:10.1017/ S0950268821001254.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.