REVIEW PAPER
Borderline ovarian tumours in pregnant and non-pregnant women – literature review
1
Katedra i Klinika Położnictwa i Perinatologii Uniwersytetu Medycznego w Lublinie, Polska
2
Doktorant Uniwersytetu Medycznego w Lublinie, Polska
3
Klinika Chorób Płuc i Reumatologii Dziecięcej Uniwersyteckiego Szpitala Dziecięcego w Lublinie, Polska
4
Bringhton and Sussex University Hospital NHS Trust, United Kingdom
5
II Katedra i Klinika Ginekologii Uniwersytetu Medycznego w Lublinie
Corresponding author
Monika Ruszała
Katedra i Klinika Położnictwa i Perinatologii Uniwersytetu Medycznego w Lublinie, Polska
Katedra i Klinika Położnictwa i Perinatologii Uniwersytetu Medycznego w Lublinie, Polska
Med Og Nauk Zdr. 2021;27(3):252-260
KEYWORDS
TOPICS
ABSTRACT
Introduction:
Borderline ovarian tumours develop most often in women under the age of 40, with latent onset and lack of specific symptoms. Due to the consequences they bring from the clinical point of view, they constitute a condition which requires considerable attention, with emphasis on pregnant women. The effect of pathological changes within the ovary on the course of pregnancy and perinatal outcomes is still a broad and up-to-date problem. Medical teams face challenges in the field of adequate diagnostics and therapy, as well as dilemmas regarding the assessment of the advantages and disadvantages of medical treatment and access to modern diagnostic methods, all of which determine the optimal medical solutions for any case.
Objective:
The aim of this review is to compare the aspects related to the occurrence of borderline ovarian tumours in pregnant and non-pregnant women based on the current literature.
Material and Methods:
A review of literature concerning the discussed problem was performed in PubMed database. The searching strategy was based on the following terms and keywords combinations: „borderline ovarian tumour”, „borderline ovarian tumour in pregnancy”, „adnexal masses”, and „ovarian tumour in pregnancy”. We considered all articles in English from January 1995 to April 2021. After applying the exclusion criteria, 71 articles were selected.
Summary:
The diagnostics of ovarian borderline tumours poses numerous difficulties and treatment methods require extensive knowledge and cooperation of various groups of specialists. Management is based on the current clinical condition of the pregnant woman, available treatment methods, gestational age, history of chronic diseases and hereditary disorders. Therapy should be selected on a case-by-case basis
Borderline ovarian tumours develop most often in women under the age of 40, with latent onset and lack of specific symptoms. Due to the consequences they bring from the clinical point of view, they constitute a condition which requires considerable attention, with emphasis on pregnant women. The effect of pathological changes within the ovary on the course of pregnancy and perinatal outcomes is still a broad and up-to-date problem. Medical teams face challenges in the field of adequate diagnostics and therapy, as well as dilemmas regarding the assessment of the advantages and disadvantages of medical treatment and access to modern diagnostic methods, all of which determine the optimal medical solutions for any case.
Objective:
The aim of this review is to compare the aspects related to the occurrence of borderline ovarian tumours in pregnant and non-pregnant women based on the current literature.
Material and Methods:
A review of literature concerning the discussed problem was performed in PubMed database. The searching strategy was based on the following terms and keywords combinations: „borderline ovarian tumour”, „borderline ovarian tumour in pregnancy”, „adnexal masses”, and „ovarian tumour in pregnancy”. We considered all articles in English from January 1995 to April 2021. After applying the exclusion criteria, 71 articles were selected.
Summary:
The diagnostics of ovarian borderline tumours poses numerous difficulties and treatment methods require extensive knowledge and cooperation of various groups of specialists. Management is based on the current clinical condition of the pregnant woman, available treatment methods, gestational age, history of chronic diseases and hereditary disorders. Therapy should be selected on a case-by-case basis
REFERENCES (71)
1.
Tavassoli F, Devilee P. Pathology and genetics of tumours of the breast and female genital organs. France IARC Press, Lyon. 2013; 4: 250.
2.
Markowska J, Jasiówka M, Szarszewska M, Blecharz P. Guzy graniczne jajnika. Ginekologia po Dyplomie 2019; 1.
3.
Vasconcelos I, Darb-Esfahani S, Sehouli J. Serous and mucinous bor-derline ovarian tumours: differences in clinical presentation, high-risk histopathological features, and lethal recurrence rates. BJOG 2016; 123(4): 498–508.
4.
Fischerova D, Zikan M, Dundr P. Diagnosis, treatment and follow-up of borderline ovarian tumors. Oncologist 2012; 17: 515–1533.
5.
Seong SJ, Kim DH, Kim MK, Song T. Controversies in Borderline Ovarian Tumors. J Gynecol Oncol 2015; 26(4): 343–349.
6.
Cosentino F, Turco LC, Cianci S, Fanfani F, Fagotti A, Alletti SG, Viz-zielli G, Vitale SG, Laganà AS, Padula F, Coco C, Pisconti S, Scambia G. Management, prognosis and reproductive outcomes of borderline ovarian tumor relapse during pregnancy: from diagnosis to potential treatment options. J Prenat Med 2016; 10(1–2): 8–14.
7.
Tropé C, Davidson B, Paulsen T. Diagnosis and treatment of borderline ovarian “the state of the art”. Eur J Gynecol Oncol 2009; 30(5): 471–482.
8.
Liu F, Hu DH, Zhang YF, Wang B, Huang K, Wang CY, Xia XY. A Retro-spective Study of Tumor and Fertility Outcomes After Fertility-Sparing Surgical Treatment of Patients with Borderline Ovarian Tumors. Zhong-hua Yi Xue Za Zhi 2017; 97(47): 3699–3703.
9.
Berek JS, Crum C, Friedlander M, Cancer of the ovary, fallopian tube, and peritoneum. Int J Gynaecol Obstet. 2015; 131(2): 111–122.
10.
BohîlŢea RE, Bacalbaşa N, Ţurcan N, Cîrstoiu MM, Terzea DC, Simion G, Munteanu O, Berceanu C, Brătilă E. Bilateral Serous Surface Pa-pillary Borderline Ovarian Tumor in 19-year-old Patient. Ultrasound, Immunohistochemical and Therapeutic Particularities of Reproductive Age. Rom J Morphol Embryol 2017; 58(3): 989–995.
11.
Yahata T, Banzai C, Tanaka K. Histology-specific long-term trends in the incidence of ovarian cancer and borderline tumor in Japanese females: a population-based study from 1983 to 2007 in Niigata, J Obstet Gynaecol Res. 2012; 38: 645–650.
12.
Daraï E, Fauvet R, Uzan C, Gouy S, Duvillard P, Morice P. Fertility and borderline ovarian tumor: a systematic review of conservative management, risk of recurrence and alternative options. Hum Reprod Update. 2013; 19(2): 151–166.
13.
Korenaga T-R K, Tewari KS. Gynecologic Cancer in Pregnancy. Gynecol Oncol 2020; 157(3): 799–809.
14.
Roy J, Babu AS. Granulosa Cell Tumor of the Ovary – An Incidental Finding During Caesarean Section – A Rare Case Report. Kathmandu Univ Med J. 2014; 12(45): 60–63.
15.
Fauvet R, Brzakowski M, Morice P, Resch B, Marret H, Graesslin O, Daraï E. Borderline ovarian tumors diagnosed during pregnancy exhibit a high incidence of aggressive features: results of a French multicenter study. Ann Oncol. 2012; 23(6): 1481–1487.
16.
Hahn U, Wallwiener D. Ovarian Tumors and Pregnancy. Zentralbl Gynakol. 1996; 118(6): 334–335.
17.
Nowak-Markwitz E, Spaczyński M. Ovarian cancer – modern approach to its origin and histogenesis. Ginekol Pol. 2012; 83: 454–457.
18.
Dubeau L. The cell origin of ovarian epithelial tumors and the ovarian surface epithelium dogma: does the emperor have no clothes? Gynecol Oncol. 1999; 72: 437–442.
19.
Shih I, Kurman R. Ovarian tumorigenesis: a proposed model based on morphological and molecular genetic analysis. Am J Pathol. 2004; 164: 1511–1518.
20.
Kindelberger D, Lee Y, Miron A. Intraepithelial carcinoma of the fimbria and pelvic serous carcimona: evidence for causal relationship. Am J Surg Pathol. 2007; 31: 161–169.
21.
Sharma A, Gentry-Maharaj A, Burnell M. Assessing the malignant potential of ovarian inclusion cycts in postmenopausal women within the UK Collaborative Trial of Ovarian Cancer Screening (UKCTOCS): a prospective cohort study. BJOG. 2012; 119: 207–219.
23.
Tashima L, Hori K, Ono H, Nagano T, Nakatsuka SI, Ito K. Endometrioid adenocarcinoma originating simultaneously from endometrium, sites of adenomyosis and ovarian endometriosis: A case report and review of our cancer database. Int J Surg Case Rep. 2017; 41: 226–229.
24.
Terry KL, Titus-Ernstoff L, McKolanis JR, Welch WR, Finn OJ, Cramer DW. Incessant ovulation, mucin 1 immunity, and risk for ovarian can-cer. Cancer Epidemiol Biomarkers Prev. 2007; 16: 30–35.
25.
Kujawa KA, Lisowska KM. Ovarian cancer – from biology to clinic. Postepy Hig Med Dosw. 2015; 69: 1275–1290.
26.
Mobeen S, Apostol R. Ovarian Cyst. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing 2020 Jan; PMID: 32809376.
27.
Schwartz N, Timor-tritsch IE, Wang E. Adnexal masses in pregnancy. Clin Obstet Gynecol 2009; 52(4): 570–585.
28.
Podsiadło B, Czech J, Czajkowska M. Przebieg ciąży, porodu oraz stan pourodzeniowy noworodka u kobiet ze współistniejącą chorobą nowotworową. Forum Położnictwa i Ginekologii 2018; 36: 13–19.
29.
Peccatori FA, Azim HA, Orecchia R. Cancer, pregnancy and fertility: ESMO Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2013; 24(6): 160–170.
30.
Anderson FA Jr, Spencer FA. Risk factors for venous thromboembolism. Circulation 2003; 107(1): 19–116.
31.
Chew HK, Wun T, Harvey D, Zhou H, White RH. Incidence of venous thromboembolism and its effect on survival among patients with com-mon cancers. Arch Intern Med. 2006; 166: 458–464.
32.
Morice P, Uzan C, Gouy S. Gynaecological cancers in pregnancy. Lancet. 2012; 379(9815): 558–569.
33.
American College of Obstetricians and Gynecologists’ Committee on Practice Bulletins: Gynecology. Practice Bulletin No. 174: Evaluation and Management of Adnexal Masses. Obstet Gynecol. 2016; 128(5): e210-e226.
34.
Brady PC, Simpson LL, Lewin SN, Smok D, Lerner JP, D'Alton ME, Herzog TJ, Wright JD. Safety of Conservative Management of Ovarian Masses During Pregnancy. J Reprod Med. 2013; 58(9–10): 377–382.
35.
Yazbek J, Raju KS, Ben-Nagi J, Holland T, Hillaby K, Jurkovic D. Accu-racy of Ultrasound Subjective ‹Pattern Recognition› for the Diagnosis of Borderline Ovarian Tumors. Ultrasound Obstet Gynecol. 2007; 29(5): 489–495.
36.
Kaijser J, Sayasneh A, Van Hoorde K. Presurgical diagnosis of adnexal tumours using mathematical models and scoring systems: a systematic review and meta-analysis. Hum Reprod. 2014; 20(3): 449–462.
37.
Silvestre L, Martins WP, Candido-dos-Reis FJ. Limitations of three--dimensional power Doppler angiography in preoperative evaluation of ovarian tumors. J Ovarian Res. 2015; 8: 47.
38.
Alcázar JL, García-Manero M, Laparte C. OP21.04: 3D power Doppler for predicting ovarian cancer in vascularized complex adnexal masses. Ultrasound Obstet Gynecol. 2006; 28: 507.
39.
Alcázar JL, Rodriguez D. Three-dimensional power Doppler vascular sonographic sampling for predicting ovarian cancer in cystic--solid and solid vascularized masses. J Ultrasound Med. 2009; 28: 275–281.
40.
Smoleń A, Stachowicz N, Czekierdowski A. Evaluating the diagnostic accuracy of ultrasonography in differential diagnosis of adnexal tumo-urs. Fam Med Prim Care Rev. 2016; 18: 340–344.
41.
Abbas AM, Sheha AM, Salem MN. Three-dimensional power Doppler ultrasonography in evaluation of adnexal masses. Middle East Fertil Soc J. 2017; 22: 241–245.
42.
Timmerman D, Van Calster B, Testa A. Predicting the risk of malig-nancy in adnexal masses based on the Simple Rules from the Inter-national Ovarian Tumor Analysis group. Am J Obstet Gynecol. 2016; 214 : 4 2 4 – 4 37.
43.
Marret H, Lhomme C, Lecuru F. Guidelines for the management of ovarian cancer during pregnancy. Eur J Obstet Gynecol Reprod Biol. 2010; 149: 18–21.
44.
American College of Obstetricians and Gynecologists Committee on Obstetric Practice: ACOG Committee Opinion Number 299. Guildlines for diagnostic imagining during pregnancy. Obstet Gynecol. 2004; 104: 647– 651.
45.
Tsikouras P, Liberis V, Galazios G, Panagiotidou C, Bouchlariotou S, Teichmann AT, Maroulis G. A Retrospective Analysis of Twenty-Eight Borderline Ovarian Tumours in Adolescent Girls. Eur J Gynecol Oncol. 2009; 30(1): 49–53.
46.
Schem C, Bauerschlag DO, Meinhold-Heerlein I, Fischer D, Friedrich M, Maass N. Benign and Borderline Tumors of the Ovary. Ther Umsch. 2007; 64(7): 369–374.
48.
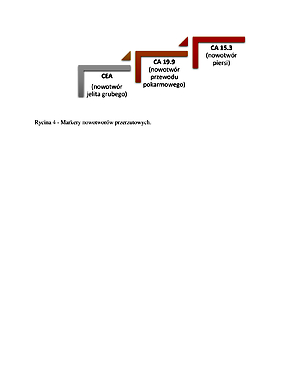
Bast RC Jr, Knapp RC. Use of the CA 125 antigen in diagnosis and monitoring of ovarian carcinoma. Eur J Obstet gynecol Reprod Biol. 1995; 129: 354–356.
49.
Santillan A, Garg R, Zahurak ML. Risk of epithelial ovarian cancer recurrence in patients with rising serum CA 125 levels within the normal range. J Clini Oncol. 2005; 23: 9338–9343.
50.
Scholler N, Garvik B, Hayden-Ledbetter M, Kline T, Urban N. Deve-lopment of a CA125-mesothelin cell adhesion assay as a screening tool for biologics discovery. Cancer Lett. 2007; 247(1): 130–136.
51.
Czekierdowski A. Nowości w diagnostyce raka jajnika. Praktyczna ultrasonografia w położnictwie i ginekologii. Wydawnictwo Exemplum, Poznań 2012; 1(4): 152–161.
52.
Montagnana M, Lippi G, Ruzzenente O. The utility of serum human epididymis protein 4 (HE4) in patients with a pelvic mass. J Clin Lab Anal 2009; 23: 331–335.
53.
Pyeon SY, Park JY, Ki KD, Lee JM. Abnormally high level of CA-19–9 in a benign ovarian cyst. Obstet Gynecol Sci. 2015; 58(6): 530–532.
54.
Szyłło K, Skrzypczak J, Skręt A. Stanowisko Zespołu Ekspertów PTG dotyczące diagnostyki i metod leczenia endometriozy. Ginekol Pol. 2012; 83: 871–876.
55.
Moore RG, Brown AK, Miller MC, Skates S, Allard WJ, Verch T. The use of multiple novel tumor biomarkers for the detection of ovarian carcino-ma in patients with a pelvic mass. Gynecol Oncol. 2007; 108: 402–408.
56.
Moore RG, McMeekin DS, Brown AK. A novel multiple marker bio-assay utilizing HE 4 and CA 125 for the prediction of ovarian cancer in patients with a pelvic mass. Gynecol Oncol. 2009; 112(1): 40–46.
57.
Dayyani F, Uhlig S, Colson B. Diagnostic performance of risk of ovarian malignancy algorithm against CA125 and HE4 in connection with ova-rian cancer: a meta-analysis. Int J Gynecol Cancer. 2016; 26: 1586–1593.
58.
Geomini P, Kruitwagen R, Bremer GL, Cnossen J, Mol BW. The accuracy of risk scores in predicting ovarian malignancy: a systematic review. Obstet Gynecol. 2009; 113: 384–394.
59.
Schmeler KM, Mayo-Smith WW, Peipert JF, Weitzen S, Manuel MD, Gordinier ME. Adnexal masses in pregnancy: surgery compared with observation. Obstet Gynecol. 2005; 105(5): 1098–1103.
60.
Leiserowitz GS. Managing Ovarian Masses During Pregnancy. Obstet Gynecol Surv. 2006; 61(7): 463–470.
61.
Morice P, Uzan C, Gouy S. Gynaecological cancers in pregnancy. Lancet. 2012; 379: 558–569.
62.
Canavan TP. Sonographic tips for evaluation of adnexal masses in pregnancy. Clin Obstet and Gynecol. 2017; 60(3): 575–585.
63.
Oliver A, Overton C. Detecting ovarian disorders in primary care. The Practicioner 2014; 258(1769): 15–19.
64.
Fruscio R, de Haan J, Van Calsteren K, Verheecke M, Mhallem M, Amant F. Ovarian cancer in pregnancy. Best Pract Res Clin Obstet Gynaecol. 2017; 41: 108–117.
65.
Tropé CG, Kaern J, Davidson B. Borderline ovarian tumours. Best Pract Res Clin Obstet Gynaecol. 2012; 26(3): 325–336.
66.
Amant F, Halaska MJ, Fumagalli M. ESGO task force ‘Cancer in Pre-gnancy’. Gynecologic cancers in pregnancy: guidelines of a second inter-national consensus meeting. Int J Gynecol Cancer. 2014; 24(3): 394–403.
67.
Song T, Choi CH, Kim H-J, Lee W, Lee Y-Y, Kim T-J, Lee J-W, Bae D-S, Kim B-G. Oncologic and Reproductive Outcomes in Patients With Advanced-Stage Borderline Ovarian Tumors. Eur J Obstet Gynecol Reprod Biol. 2011; 60(3): 204–208.
68.
Rubach M, Mądry R, Wełnicka-Jaśkiewicz M. Nowotwory w ciąży. Za-lecenia postępowania diagnostyczno-terapeutycznego w nowotworach złośliwych. Via Medica, Gdańsk. 2013; 4(2): 68–85.
69.
Borgfeldt C, Iosif C, Måsbäck A. Fertility-sparing Surgery and Outcome in Fertile Women With Ovarian Borderline Tumors and Epithelial Invasive Ovarian Cancer. Eur J Obstet Gynecol Reprod Biol. 2007; 134(1): 110 –114.
70.
Cosyns S, De Sutter P, Tournaye H. Necessity of appendectomy for mucinous borderline ovarian tumors. Systematic review. Arch Gynecol Obstet. 2016; 294(6): 1283–1289.
71.
Semczuk A, Gogacz M, Semczuk-Sikora A, Jóźwik M, Rechberger T. The Putative Role of TP53 Alterations and p53 Expression in Borderline Ovarian Tumors – Correlation with Clinicopathological Features and Prognosis: A Mini-Review. J Cancer. 2017; 8(14): 2684–2691.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.