RESEARCH PAPER
Dietary factors and glycaemic control in patients with diabetes
1
Chair of Human Nutrition and Dietetics, University of Life Sciences, Poznań, Poland
Corresponding author
Karolina Łagowska
Department of Human Nutrition and Dietetics, Poznań University of Life Sciences, Wojska Polskiego 31, 60-624 Poznań, Poland
Department of Human Nutrition and Dietetics, Poznań University of Life Sciences, Wojska Polskiego 31, 60-624 Poznań, Poland
Med Og Nauk Zdr. 2025;31(3):185-191
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Although type 1 and type 2 diabetes differ significantly in various aspects, including etiology, treatment and medical guidelines, does the type of disease influence the level of management? The aim of the study is to identify the differences in BMI, food frequency intake, and levels of physical activity between individuals with different types of diabetes, and to assess the link between dietary factors and HbA1c levels.
Material and methods:
The study included 78 patients (mean age 42.8 ± 18.2 years), with T1D (n= 49) or T2D (n= 29). Patients were categorized also into two groups: with higher level of HbA1c (> 6.5%, n = 67) and normal level of HbA1c (<6.5% n = 11). The KomPAN questionnaire, supplemented with additional diabetes-related questions, were completed by each participant.
Results:
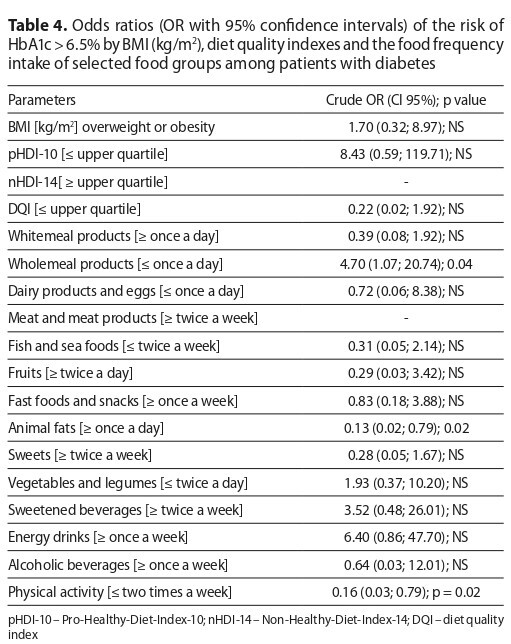
T1D was associated with younger age, lower BMI and worse dietary habits, compared to T2D. Higher dietary quality index scores were observed among women with T1D, compared to men, and lower consumption of meat and meat products was reported. Greater levels of physical activity were reported by patients with normal HbA1c. Higher HbA1c level (> 6.5%) was linked to consuming animal fats more than once daily and whole meal products less than once daily.
Conclusions:
Food frequency intake and diet quality may be dependent on the type of diabetes and gender. Appropriate HbA1c levels may be connected not only with proper dietary habits, but also with physical activity. The study, however, has significant limitations, including the heterogeneity of the groups; therefore, it is necessary for further research to be conducted on more homogenous populations.
Although type 1 and type 2 diabetes differ significantly in various aspects, including etiology, treatment and medical guidelines, does the type of disease influence the level of management? The aim of the study is to identify the differences in BMI, food frequency intake, and levels of physical activity between individuals with different types of diabetes, and to assess the link between dietary factors and HbA1c levels.
Material and methods:
The study included 78 patients (mean age 42.8 ± 18.2 years), with T1D (n= 49) or T2D (n= 29). Patients were categorized also into two groups: with higher level of HbA1c (> 6.5%, n = 67) and normal level of HbA1c (<6.5% n = 11). The KomPAN questionnaire, supplemented with additional diabetes-related questions, were completed by each participant.
Results:
T1D was associated with younger age, lower BMI and worse dietary habits, compared to T2D. Higher dietary quality index scores were observed among women with T1D, compared to men, and lower consumption of meat and meat products was reported. Greater levels of physical activity were reported by patients with normal HbA1c. Higher HbA1c level (> 6.5%) was linked to consuming animal fats more than once daily and whole meal products less than once daily.
Conclusions:
Food frequency intake and diet quality may be dependent on the type of diabetes and gender. Appropriate HbA1c levels may be connected not only with proper dietary habits, but also with physical activity. The study, however, has significant limitations, including the heterogeneity of the groups; therefore, it is necessary for further research to be conducted on more homogenous populations.
REFERENCES (38)
1.
Petersmann A, Müller-Wieland D, Müller UA, et al. Definition, Classification and Diagnosis of Diabetes Mellitus. Exp Clin Endocrinol Diabetes. 2019;127:1–7. doi:10.1055/a-1018-9078.
2.
ElSayed NA, Aleppo G, Aroda VR, et al. 2. Classification and Diagnosis of Diabetes: Standards of Care in Diabetes—2023. Diabetes Care. 2023;46:19–40. doi:10.2337/dc23-S002.
3.
Roep BO, Thomaidou S, van Tienhoven R, et al. Type 1 diabetes mellitus as a disease of the β-cell (do not blame the immune system?). Nat Rev Endocrinol. 2021;17(3):150–61. doi:10.1038/s41574-020-00443-4.
4.
Marcus C, Danielsson P, Hagman E. Pediatric obesity—Long-term consequences and effect of weight loss. J Intern Med. 2022;292(6):870–91. doi:10.1111/joim.13547.
5.
Redondo MJ, Hagopian WA, Oram R, et al. The clinical consequences of heterogeneity within and between different diabetes types. Diabetologia. 2020;63(10):2040–8. doi:10.1007/s00125-020-05211-7.
6.
Evert AB, Dennison M, Gardner CD, et al. Nutrition Therapy for Adults With Diabetes or Prediabetes: A Consensus Report. Diabetes Care. 2019;42(5):731–54. doi:10.2337/dci19-0014.
7.
Araszkiewicz A, Borys S, Broncel M, et al. 2025 Guidelines on the management of patients with diabetes – a position of Diabetes Poland. Curr Topics Diabet. 2025;5:1–158. doi.org/10.5114/ctd/203685.
8.
The Diabetes and Nutrition Study Group (DNSG) of the European Association for the Study of Diabetes (EASD), Aas AM, Axelsen M, Churuangsuk C, et al. Evidence-based European recommendations for the dietary management of diabetes. Diabetologia. 2023;66(6):965–85. doi:10.1007/s00125-023-05894-8.
9.
Cole JB, Florez JC. Genetics of diabetes mellitus and diabetes complications. Nat Rev Nephrol. 2020;16(7):377–90. doi:10.1038/s41581-020-0278-5.
10.
Geng T, Zhu K, Lu Q, et al. Healthy lifestyle behaviors, mediating biomarkers, and risk of microvascular complications among individuals with type 2 diabetes: A cohort study. PLoS Med. 2023;20:e1004135. doi:10.1371/journal.pmed.1004135.
11.
Jaworski M, Panczyk M, Cedro M, et al. Adherence to dietary recommendations in diabetes mellitus: disease acceptance as a potential mediator. Patient Prefer Adher. 2018;12:163–74. doi:10.2147/PPA.S147233.
12.
Kowalkowska J, Wadolowska L, Czarnocinska J, et al. Reproducibility of a Questionnaire for Dietary Habits, Lifestyle and Nutrition Knowledge Assessment (KomPAN) in Polish Adolescents and Adults. Nutrients 2018;10:1845. doi:10.3390/nu10121845.
13.
Kodama S, Horikawa C, Fujihara K, et al. Quantitative relationship between body weight gain in adulthood and incident type 2 diabetes: a meta‐analysis. Obes Rev. 2014;15(3):202–14. doi:10.1111/obr.12129.
14.
Nagaya T, Yoshida H, Takahashi H, et al. Increases in body mass index, even within non-obese levels, raise the risk for Type 2 diabetes mellitus: a follow-up study in a Japanese population. Diabet Med. 2005;22(8):1107–11. doi:10.1111/j.1464-5491.2005.01602.x.
15.
Kaneto C, Toyokawa S, Miyoshi Y, et al. Long-term weight change in adulthood and incident diabetes mellitus: MY Health Up Study. Diabetes Res Clin Pract. 2013;102(2):138–46. doi:10.1016/j.diabres.2013.08.011.
16.
Richardson Tg, Crouch DJM, Power GM, et al. Childhood body size directly increases type 1 diabetes risk based on a lifecourse Mendelian randomization approach. Nat Commun. 2022;13;2337. doi.org/10.1038/s41467-022-29932-y.
17.
Censin JC, Nowak Ch, Cooper N, et al. Childhood adiposity and risk of type 1 diabetes: Amendelian randomization study. PLoS Med. 2017;14(8):e1002362; doi.org/10.1371/journal.pmed.1002362.
18.
Hyppönen E, Virtanen SM, Kenward MG, et al. Childhood Diabetes in Finland Study Group. Obesity, increased linear growth, and risk of type 1 diabetes in children. Diabetes Care. 2000;23:1755–60. doi:10.2337/diacare.23.12.1755.
19.
Feraco A, Armani A, Amoah I, et al. Assessing gender differences in food preferences and physical activity: a population-based survey. Front Nutr. 2024;20:1348456. doi:10.3389/fnut.2024.1348456.
20.
Piłaciński S, Zozulińska-Ziółkiewicz DA. Influence of lifestyle on the course of type 1 diabetes mellitus. Arch Med Sci. 2014;24;10(1):124–34. doi:10.5114/aoms.2014.40739.
21.
AlBurno H, Mercken L, de Vries H, et al. Determinants of healthful eating and physical activity among adolescents and young adults with type 1 diabetes in Qatar: A qualitative study. PLoS One. 2022;6;17(7):e0270984. doi:10.1371/journal.pone.0270984.
22.
Micha R, Mozaffarian D. Trans fatty acids: effects on metabolic syndrome, heart disease and diabetes. Nat Rev Endocrinol. 2009;5(6):335–44. doi:10.1038/nrendo.2009.79.
23.
Wolpert HA, Anderson BJ. Young adults with diabetes: need for a new treatment paradigm. Diabetes Care. 2001;24(9):1513–4. doi:10.2337/diacare.24.9.1513.
24.
Morinaka T, Wozniewicz M, Jeszka J, et al. Westernization of dietary patterns among young Japanese and Polish females – a comparison study. Ann Agric Environ Med. 2013;20(1):122–30. doi:10.1038/nrendo.2009.79.
25.
Bleich SN, Wang YC. Consumption of Sugar-Sweetened Beverages Among Adults With Type 2 Diabetes. Diabetes Care. 2011;34:551–5. doi:10.2337/dc10-1687.
26.
Olateju T, Begley J, Green DJ, et al. Physiological and Glycemic Responses Following Acute Ingestion of a Popular Functional Drink in Patients with Type 1 Diabetes. Can J Diabetes. 2015;39:78–82. doi:10.1016/j.jcjd.2014.07.220.
27.
Malik VS, Popkin BM, Bray GA, et al. Sugar-Sweetened Beverages and Risk of Metabolic Syndrome and Type 2 Diabetes. Diabetes Care. 2010;33:2477–83. doi:10.2337/dc10-1079.
28.
Araszkiewicz A, Bandurska-Stankiewicz E, Borys S, et al. 2023 Guidelines on the management of patients with diabetes – a position of Diabetes Poland. Curr Topics Diabet. 2023;3:1–133. doi:10.5114/ctd/160061.
29.
Katsarou A, Gudbjörnsdottir S, Rawshani A, et al. Type 1 diabetes mellitus. Nat Rev Dis Primers. 2017;3:17016. doi:10.1038/nrdp.2017.16.
30.
Critchley JA, Carey IM, Harris T et al. Variability in Glycated Haemaglobin and Risk of Poor Outcomes Among People With Type 2 Diabetes in a Large Primary Care Cohort Study. Diabetes Care. 2019;42:2237–46. doi:10.2337/dc19-0848.
31.
Bergenstal RM. Glycemic Variability and Diabetes Complications: Does It Matter? Simply Put, There Are Better Glycemic Markers!. Diabetes Care. 2015;38:1615–21. doi:10.2337/dc15-0099.
32.
Sugimoto T, Sakurai T, Uchida K, et al. Impact of Type 2 Diabetes and Glycated Haemaglobin Levels Within the Recommended Target Range on Mortality in Older Adults With Cognitive Impairment Receiving Care at a Memory Clinic: NCGG-STORIES. Diabetes Care. 2024;47:864–72. doi:10.2337/dc23-2324.
33.
Olesen KKW, Thrane PG, Hansen MK, et al. The impact of glycated haemaglobin A1c on cardiovascular risk in diabetes patients with and without coronary artery disease. Eur Heart J. 2023;44:ehad655.2546. doi:10.1056/NEJMoa0908359.
34.
Grahovac M, Kumric M, Vilovic M, et al. Adherence to Mediterranean diet and advanced glycation endproducts in patients with diabetes. World J Diabetes. 2021;12(11):1942–56. doi:10.4239/wjd.v12.i11.1942.
35.
Benson G, Hayes J. An Update on the Mediterranean, Vegetarian, and DASH Eating Patterns in People With Type 2 Diabetes. Diabetes Spectr. 2020;33:125–32. doi:10.2337/ds19-0073.
36.
Swartz AM, Strath SJ, Bassett DR, et al. Increasing daily walking improves glucose tolerance in overweight women. Prev Med. 2003;37(4):356–62. doi:10.1016/s0091-7435(03)00144-0.
37.
Messina G, Alioto A, Parisi MC, et al. Experimental study on physical exercise in diabetes: pathophysiology and therapeutic effects. Eur J Transl Myol. 2023;33(4):11560. doi:10.4081/ejtm.2023.11560.
38.
Charles D, Sabouret P, Moll A, et al. The relationship between mortality and daily number of steps in type 2 diabetes. Panminerva Med. 2023;65(3):335–42. doi:10.23736/S0031-0808.22.04732-2.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.