RESEARCH PAPER
Analiza wielokierunkowa czynników towarzyszących nadwadze i otyłości u dzieci i młodzieży – badanie przekrojowe
1
Department of Nutrition in Digestive Tract Diseases, Medical University of Lodz, Łódź, Poland
2
Regional Centre for Rare Diseases, Polish Mother’s Memorial Hospital Research Institute, Łódź, Poland
3
Department of Paediatrics and Allergy, Copernicus Memorial Hospital, Łódź, Poland
4
Department of Paediatrics, Immunology, Nephrology, Polska
5
Department of Hygiene and Health Promotion, Medical University of Lodz, Łódź, Poland
Corresponding author
Aneta Gwozdowska
Department of Nutrition in Digestive Tract Diseases, Rzgowska 281/289, 93-338 Łódż, Poland
Department of Nutrition in Digestive Tract Diseases, Rzgowska 281/289, 93-338 Łódż, Poland
Med Og Nauk Zdr. 2023;29(1):39-45
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Overweight and obesity in children and adolescents has been one of the major health and social challenges worldwide for several decades. Obesity is a multifactorial disease in which the risk factors may appear with various severity and combinations. The aim of the study was to identify associated factors for childhood obesity and conduct a multivariate analysis.
Material and methods:
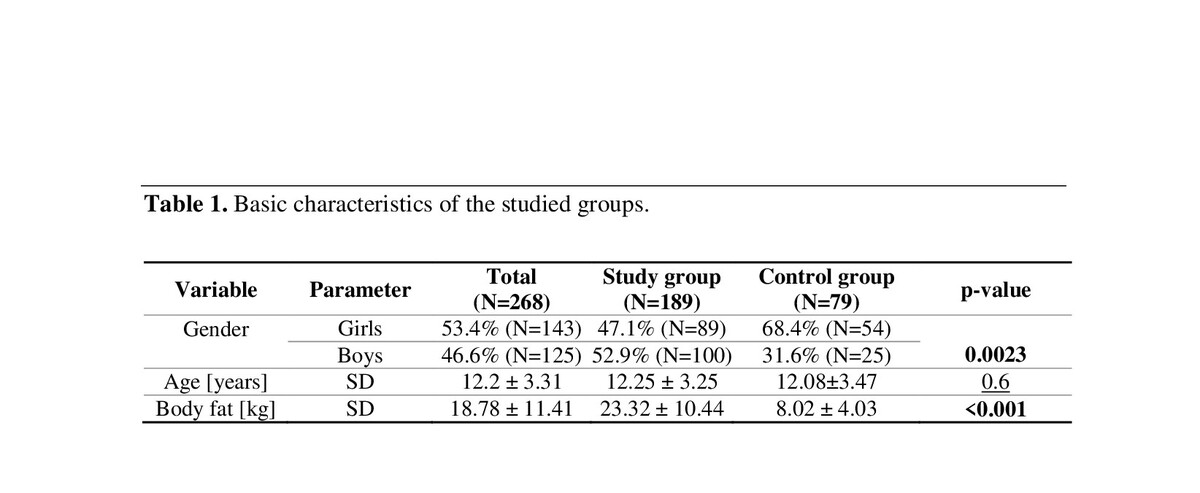
The study included a group of 268 schoolchildren and adolescents. The children were assigned to one of two groups: study group – children with overweight and obese, and control group – children with normal weight. Data were collected using questionnaires related to prenatal, biological, environmental, behavioural, and nutritional risk factors for obesity.
Results:
Of the examined factors, six proved to be significantly associated with the risk of developing childhood overweight or obesity: gender (<0.05), maternal pre-pregnancy BMI (p < 0.001), maternal BMI (<0.001), lower socio-economic status (SES) (p <0.05), waking time at weekends (p <0.05), and snacking between meals (p <0.05). The results of the multivariate analysis indicate that the chance of a child being overweight or obese was over 6.5 twice as likely if the mother was overweight or obese (OR = 6.564; p <0.001). Male children were approximately twice more likely to become obese or overweight than female children (OR = 2.199; < 0.05). The risk of excess weight was 2.5 times higher in children who ate between meals than in the rest of the group (OR = 2.514; p < 0.05).
Conclusions:
Factors related to the mother, and not both parents, have a stronger impact on the development of overweight and obesity in children. Women`s excess body weight at pre-pregnancy is the most significant factor influencing the child`s future high body weight.
Overweight and obesity in children and adolescents has been one of the major health and social challenges worldwide for several decades. Obesity is a multifactorial disease in which the risk factors may appear with various severity and combinations. The aim of the study was to identify associated factors for childhood obesity and conduct a multivariate analysis.
Material and methods:
The study included a group of 268 schoolchildren and adolescents. The children were assigned to one of two groups: study group – children with overweight and obese, and control group – children with normal weight. Data were collected using questionnaires related to prenatal, biological, environmental, behavioural, and nutritional risk factors for obesity.
Results:
Of the examined factors, six proved to be significantly associated with the risk of developing childhood overweight or obesity: gender (<0.05), maternal pre-pregnancy BMI (p < 0.001), maternal BMI (<0.001), lower socio-economic status (SES) (p <0.05), waking time at weekends (p <0.05), and snacking between meals (p <0.05). The results of the multivariate analysis indicate that the chance of a child being overweight or obese was over 6.5 twice as likely if the mother was overweight or obese (OR = 6.564; p <0.001). Male children were approximately twice more likely to become obese or overweight than female children (OR = 2.199; < 0.05). The risk of excess weight was 2.5 times higher in children who ate between meals than in the rest of the group (OR = 2.514; p < 0.05).
Conclusions:
Factors related to the mother, and not both parents, have a stronger impact on the development of overweight and obesity in children. Women`s excess body weight at pre-pregnancy is the most significant factor influencing the child`s future high body weight.
REFERENCES (30)
1.
Lobstein T, Jackson-Leach R, Moodie ML, et al. Child and adolescent obesity: Part of a bigger picture. Lancet. 2015;385(9986):2510–2520. doi:10.1016/S0140-6736(14)61746-3.
2.
UNICEF, WHO, and World Bank, Levels and trends in child malnutrition: Key findings of the 2020 Edition of the Joint Child Malnutrition Estimates. WHO. 2020;24(2):1–16. doi:10.18356/6ef1e09a-en.
3.
WHO Europe Region, Childhood Obesity Surveillance Initiative (COSI) Report on the fifth round of data collection 2018–2020. WHO Region 2020;1:1–88.
4.
Simmonds M, Llewellyn A, Owen CG, et al. Predicting adult obesity from childhood obesity: A systematic review and meta-analysis. Obes Rev. 2016;17(2):95–107. doi:10.1111/obr.12334.
5.
Kumar S, Kelly AS, Review of Childhood Obesity: From Epidemiology, Etiology, and Comorbidities to Clinical Assessment and Treatment. Mayo Clin Proc. 2017;92(2):251–265. doi:10.1016/j.mayocp.2016.09.017.
6.
Llewellyn A, Simmonds M, Owen CF, et al. Childhood obesity as a predictor of morbidity in adulthood: a systematic review and meta-analysis. Obes Rev. 2016;7(1):56–67. doi:10.1111/obr.12316.
7.
Woo Baidal JA, Locks LM, Cheng ER, et al. Risk Factors for Childhood Obesity in the First 1,000 Days: A Systematic Review. Am J Prev Med. 2016;50(6):761–779. doi:10.1016/j.amepre.2015.11.012.
8.
Larqué E, Labayen I, Flodmark CE, et al. From conception to infancy – early risk factors for childhood obesity. Nat Rev Endocrinol. 2019; 15(8):456–478. doi:10.1038/s41574-019-0219-1.
9.
Gray HL, Buro AW, Barrera Ikan J, et al. School-level factors associated with obesity: A systematic review of longitudinal studies. Obes Rev. 2019;20(7):1–17. doi:10.1111/obr.12852.
10.
Bates CR, Buscemi J, Nicholson LM, et al. Links between the organization of the family home environment and child obesity: a systematic review. Obes Rev. 2018;19(5):716–727. doi:10.1111/obr.12662.
11.
Wang J, Wu Y, Xiong G, et al. Introduction of complementary feeding before 4 months of age increases the risk of childhood overweight or obesity: A meta-analysis of prospective cohort studies. Nutr Res. 2016;36(8):759–770. doi:10.1016/j.nutres.2016.03.003.
12.
Liberali R, Kupek E, Altenburg de Assis MA, Dietary Patterns and Childhood Obesity Risk: A Systematic Review. Child Obes. 2020;16(2):70–85. doi:10.1089/chi.2019.0059.
13.
Porter RM, Tindal A, Gaffka BJ, et al. A Review of Modifiable Risk Factors for Severe Obesity in Children Ages 5 and under. Child Obes. 2018;14(7):468–476. doi:10.1089/chi.2017.0344.
14.
Albuquerque D, Nóbrega C, Manco L, et al. The contribution of genetics and environment to obesity. Br Med Bull. 2017;123(1):159–173. doi:10.1093/bmb/ldx022.
15.
Talma H, Chinapaw MJM, Bakker B, et al. Bioelectrical impedance analysis to estimate body composition in children and adolescents: a systematic review and evidence appraisal of validity, responsiveness, reliability and measurement error. Obes Rev. 2013;14(11):895–905. doi:10.1111/obr.12061.
16.
Kułaga Z, Różdżyńska-Świątkowska A, Grajda A, et al. Siatki centylowe dla oceny wzrastania i stanu odżywienia polskich dzieci i młodzieży od urodzenia do 18 roku życia [Percentile charts for growth and nutritional status assessment in Polish children and adolescents from birth to 18 year of age]. Stand Med Pediatr. 2015;12:119–134.
17.
I. of medicine and N. R. Council, Composition and Components of Gestational Weight Gain: Physiology and Metabolism in Weight gain during pregnancy: Reexamining the guidelines. The National Academies Press. 2009:71–110.
18.
Paruthi S, Brooks LJ, D’Ambrosio C, et al. Recommended amount of sleep for pediatric populations: A consensus statement of the American Academy of Sleep Medicine. J Clin Sleep Med. 2016;12(6):785–786. doi:10.5664/jcsm.5866.
19.
Greydanus DE, Agana M, Kamboj MK, et al. Pediatric obesity: Current concepts. Dis Mon. 2018;64(4):98–156. doi:10.1016/j.disamonth.2017.12.001.
20.
Bammann K, Peplies J, De Henauw S, et al. Early Life Course Risk Factors for Childhood Obesity: The IDEFICS Case-Control Stud. PLoS One. 2014;9(2):e86914. doi:10.1371/journal.pone.0086914.
21.
Voerman E, Santos S, Golab BP, et al. Maternal body mass index, gestational weight gain, and the risk of overweight and obesity across childhood: An individual participant data meta-analysis. PLoS Med. 2019;16(2):e1002744. doi:10.1371/journal.pmed.1002744.
22.
Williams CB, MacKenzie KC, Gahagan S, The effect of maternal obesity on the offspring. Clin Obstet Gynecol. 2014;57(3):508–515. doi:10.1097/GRF.0000000000000043.
23.
Linabery AM, Nahhas RW, Johnson W, et al. Stronger influence of maternal than paternal obesity on infant and early childhood body mass index: The Fels Longitudinal Study. Pediatr Obes. 2013;8(3):159–169. doi:10.1111/j.2047-6310.2012.00100.x.
24.
Rogers R, Eagle TF, Sheetz A, et al. The Relationship between Childhood Obesity, Low Socioeconomic Status, and Race/Ethnicity: Lessons from Massachusetts. Child Obes. 2015;11(6):691–695. doi:10.1089/chi.2015.0029.
25.
Fatima Y, Doi SA, and Mamun AA, Sleep quality and obesity in young subjects: a meta-analysis. Obes Rev. 2016;17(11):1154–1166. doi:10.1111/jpc.13434.
26.
Li L, Zhang S, Huang Y, et al. Sleep duration and obesity in children: A systematic review and meta-analysis of prospective cohort studies. J Paediatr Child Health. 2017;53(4):378–385. doi:10.1111/jpc.13434.
27.
Skjåkødegård HF, Danielsen YS, et al. Beyond sleep duration: Sleep timing as a risk factor for childhood obesity. Pediatr Obes. 2020;e12698: 1–11. doi:10.1111/ijpo.12698.
28.
Nicklas TA, Baranowski T, Cullen KW, et al. Eating patterns, dietary quality and obesity. J Am Coll Nutr. 2001;20(6):599–608. doi:10.1080/07315724.2001.10719064.
29.
Koletzko B, Toschke AM, Meal patterns and frequencies: Do they affect body weight in children and adolescents? Crit Rev Food Sci Nutr. 2010;50(2):100–105. doi:10.1080/10408390903467431.
30.
Maffeis C, Grezzani A, Perrone L, et al. Could the savory taste of snacks be a further risk factor for overweight in children? J Pediatr Gastroenterol Nutr. 2008;46(4):429–37. doi:10.1097/MPG.0b013e318163b850.
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.