REVIEW PAPER
Physiological and pathological tongue conditions – the role of endogenous and exogenous factors
1
Katedra i Zakład Patologii Jamy Ustnej, Uniwersytet Medyczny im. Piastów Śląskich we Wrocławiu
Corresponding author
Polina Zalewska
Katedra I Zakład Patologii Jamy Ustnej, Uniwersytet Medyczny im. Piastów Śląskich we Wrocławiu
Katedra I Zakład Patologii Jamy Ustnej, Uniwersytet Medyczny im. Piastów Śląskich we Wrocławiu
Med Og Nauk Zdr. 2021;27(4):407-413
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
The tongue is considered to be a valuable source of information about patient’s general health, and it can also be an indicator of the presence or development of both local and general diseases. High frequency of occurrence and wide variety of the clinical presentations of the pathological tongue conditions result from its specific anatomical and histological structure. Multifactorial etiology of the tongue lesions and non-specificity of symptoms reported by the patients make it difficult to establish a correct medical diagnosis. The aim of the study is to present the most common tongue lesions, and to broaden knowledge of all medical specialists concerning the specific and non-specific tongue changes that can occur under the influence of local or general factors.
Brief description of the state of knowledge:
Among all tongue lesions, the most common are lingual atrophic conditions that often result from underlying systemic pathology. The subsequent group includes tongue disorders that are described as specific lesions of different etiology: congenital or developmental, infectious or neoplastic, or have no clearly defined etiology.
Summary:
The ability to identify benign tongue conditions and pathological tongue lesions is the key in making the correct diagnosis and initiating the effective treatment without iatrogenic damage. Proper diagnosis and management of tongue conditions can reduce patient anxiety associated with the presence of tongue lesions, and significantly improve patient’s quality of life.
The tongue is considered to be a valuable source of information about patient’s general health, and it can also be an indicator of the presence or development of both local and general diseases. High frequency of occurrence and wide variety of the clinical presentations of the pathological tongue conditions result from its specific anatomical and histological structure. Multifactorial etiology of the tongue lesions and non-specificity of symptoms reported by the patients make it difficult to establish a correct medical diagnosis. The aim of the study is to present the most common tongue lesions, and to broaden knowledge of all medical specialists concerning the specific and non-specific tongue changes that can occur under the influence of local or general factors.
Brief description of the state of knowledge:
Among all tongue lesions, the most common are lingual atrophic conditions that often result from underlying systemic pathology. The subsequent group includes tongue disorders that are described as specific lesions of different etiology: congenital or developmental, infectious or neoplastic, or have no clearly defined etiology.
Summary:
The ability to identify benign tongue conditions and pathological tongue lesions is the key in making the correct diagnosis and initiating the effective treatment without iatrogenic damage. Proper diagnosis and management of tongue conditions can reduce patient anxiety associated with the presence of tongue lesions, and significantly improve patient’s quality of life.
REFERENCES (32)
1.
Haller JS. The foul tongue: a 19th century index of disease. West J Med.1982; 137: 258–64.
2.
Edwards M. Put out your tongue! The role of clinical insight in the study of the history of medicine. Med Hist. 2011; 55: 301–6. https://doi.org/10.1017/S00257....
3.
Chiang CP, Chang JYF, Wang YP, Wu YH, Wu YC, Sun A. Atrophic glossitis: Etiology, serum autoantibodies, anemia, hematinic deficien-cies, hyperhomocysteinemia, and management. J Formos Med Assoc. 2020; 119: 774–80. https://doi.org/10.1016/j.jfma....
4.
Reamy B V, Derby R, Col LT. Common Tongue Conditions in Primary Care – American Family Physician. Am Fam Physician. 2010; 81: 627–34.
5.
Kimori H, Yamamoto K, Yamachika S, Tsurumoto A, Kamikawa Y, Sasao M, et al. Factors associated with the presence of atrophic tongue in patients with dry mouth. Gerodontology. 2015; 32: 13–7. https://doi.org/10.1111/ger.12....
6.
Erriu M, Pili FMG, Cadoni S, Garau V. Diagnosis of Lingual Atrophic Conditions: Associations with Local and Systemic Factors. A Descriptive Review. Open Dent J. 2016; 10: 619–35. https://doi.org/10.2174/187421....
7.
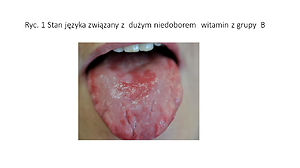
Stoopler ET, Kuperstein AS. Glossitis secondary to vitamin B12 deficiency anemia. Can Med Assoc J. 2013; 185: E582–E582. https://doi.org/10.1503/cmaj.1....
8.
Muhvić-Urek M, Tomac-Stojmenović M, Mijandrusic-Sincic B. Oral pathology in inflammatory bowel disease. World J Gastroenterol. 2016; 22: 5655–67. https://doi.org/10.3748/wjg.v2....
9.
Gupta S, Sinha N, Swarup N, Sagolsem C, Chowdhary Z. Atrophic Glossitis: Burning Agony of Nutritional Deficiency Anemia. World J Anemia. 2017; 1: 48–50. https://doi.org/10.5005/jp-jou....
10.
Samad A, Mohan N, Balaji RVS, Augustine D, Patil SG. Oral manifestations of plummer-vinson syndrome: a classic report with literature review. J Int Oral Heal JIOH. 2015; 7: 68–71.
11.
Erriu M, Canargiu F, Orrù G, Garau V, Montaldo C. Idiopathic atrophic glossitis as the only clinical sign for celiac disease diagnosis: A case report. J Med Case Rep. 2012; 6: 2–4. https://doi.org/10.1186/1752-1....
12.
Petruzzi M, Lucchese A, Campus G, Crincoli V, Lauritano D, Baldoni E. Oral stigmatic lesions of gastroesophageal reflux disease (GERD): Informe de un caso. Rev Med Chil. 2012; 140: 915–8. https://doi.org/10.4067/s0034-....
13.
Nakamura S, Okamoto MR, Yamamoto K, Tsurumoto A, Yoshino Y, Iwabuchi H, et al. The Candida species that are important for the development of atrophic glossitis in xerostomia patients. BMC Oral Health. 2017; 17: 153. https://doi.org/10.1186/s12903....
14.
Muñoz C, Martínez A, Flores M, Catalán A. Relationship Between Xerostomia and Hyposalivation in Senior Chilean People. Rev Clínica Periodoncia, Implantol y Rehabil Oral. 2019; 12: 123–6. https://doi.org/10.4067/s0719-....
15.
Serrano J, Lopez-Pintor RM, Gonzalez-Serrano J, Fernandez-Castro M, Casanas E, Hernandez G. Oral lesions in Sjogren’s syndrome: A systematic review. Med Oral Patol Oral Cir Bucal. 2018; 23: e391–400. https://doi.org/10.4317/medora....
16.
Rohani B. Oral manifestations in patients with diabetes mellitus. World J Diabetes. 2019; 10: 485–9. https://doi.org/10.4239/wjd.v1....
17.
da Cunha SF de C, de Melo DA, Braga CBM, Vannucchi H, da Cunha DF. Papillary atrophy of the tongue and nutritional status of hospitalized alcoholics. An Bras Dermatol. 2012; 87: 84–9. https://doi.org/10.1590/s0365-....
18.
Kim J, Kim MJ, Kho HS. Oral manifestations in vitamin B12 deficiency patients with or without history of gastrectomy. BMC Oral Health. 2016; 16: 1–9. https://doi.org/10.1186/s12903....
19.
Gurvits GE, Tan A. Black hairy tongue syndrome. World J Gastroen-terol. 2014; 20: 10845–50. https://doi.org/10.374/wjg.v20....
20.
Schlager E, St. Claire C, Ashack K, Khachemoune A. Black Hairy Tongue: Predisposing Factors, Diagnosis, and Treatment. Am J Clin Dermatol. 2017; 18: 563–9. https://doi.org/10.1007/s40257....
21.
Ren J, Zheng Y, Du H, Wang S, Liu L, Duan W, et al. Antibiotic-induced black hairy tongue: two case reports and a review of the literature. J Int Med Res. 2020; 48. https://doi.org/10.1177/030006....
22.
Vinod K, Reddy P, Pillai V. Scalloped tongue: A rare finding in nocturnal bruxism. Natl Med J India. 2017; 30: 296. https://doi.org/10.4103/0970--....
23.
Tomooka K, Tanigawa T, Sakurai S, Maruyama K, Eguchi E, Nishioka S, et al. Scalloped tongue is associated with nocturnal intermittent hypoxia among community-dwelling Japanese: the Toon Health Study. J Oral Rehabil. 2017; 44: 602–9. https://doi.org/10.1111/joor.1....
24.
Ogueta CI, Ramírez PM, Jiménez OC, Cifuentes MM. Geographic Tongue: What a Dermatologist Should Know. Actas Dermosifiliogr. 2019; 110: 341–6. https://doi.org/10.1016/j.ad.2....
25.
de Campos WG, Esteves CV, Fernandes LG, Domaneschi C, Júnior CAL. Treatment of symptomatic benign migratory glossitis: a systematic review. Clin Oral Investig. 2018; 22: 2487–93. https://doi.org/10.1007/s00784....
26.
Dafar A, Çevik-Aras H, Robledo-Sierra J, Mattsson U, Jontell M. Factors associated with geographic tongue and fissured tongue. Acta Odontol Scand. 2016; 74: 210–6. https://doi.org/10.3109/000163....
27.
Casu C, Viganò L. Particular shape of the tongue and benign migra-tory glossitis. Pan Afr Med J. 2018; 30: 8688. https://doi.org/10.11604/pamj.....
28.
Järvinen J, Mikkonen JJW, Kullaa AM. Fissured tongue: A sign of tongue edema? Med Hypotheses. 2014; 82: 709–12. https://doi.org/10.1016/j.mehy....
29.
Feil ND, Filippi A. Frequency of fissured tongue as a function of age. Swiss Dent J. 2016; 126: 886–91.
30.
Goregen M, Miloglu O, Buyukkurt MC, Caglayan F, Aktas AE. Median rhomboid glossitis: A clinical and microbiological study. Eur J Dent. 2011; 5: 367–72. https://doi.org/10.1055/s-0039....
31.
Panta P, Erugula SR. Median rhomboid glossitis-developmental or candidal? Pan Afr Med J. 2015; 21: 8688. https://doi.org/10.11604/pamj.....
32.
Pili FMG, Erriu M, Piras A, Garau V. Application of the novel method in the diagnosis and treatment of median rhomboid glossitis Candida-associated. Eur J Dent. 2014; 8: 129–31. https://doi.org/10.4103/1305-7....
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.