REVIEW PAPER
Problems of infection with Neisseria gonorrhoeae
1
Katedra i Zakład Mikrobiologii Lekarskiej, Warszawski Uniwersytet Medyczny, Polska
Corresponding author
Szymon Jerzy Walter de Walthoffen
Katedra i Zakład Mikrobiologii Lekarskiej, Warszawski Uniwersytet Medyczny, Tytusa Chałubińskiego 5, 02-004, Warszawa, Polska
Katedra i Zakład Mikrobiologii Lekarskiej, Warszawski Uniwersytet Medyczny, Tytusa Chałubińskiego 5, 02-004, Warszawa, Polska
Med Og Nauk Zdr. 2021;27(2):134-138
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Sexually transmitted infections are a serious public health problem worldwide, negatively affect the quality of life and cause serious diseases. More than a million sexually transmitted diseases are acquired every day. Despite the high incidence of sexually transmitted diseases, these diseases still remain a neglected area for prevention programmes, diagnostic tests and appropriate treatment. The aim of the study is presentation of the problems associated with Neisseria gonorrhoeae infections
Current state of knowledge:
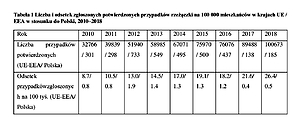
One of the most common sexually transmitted diseases is gonorrhea, caused by the bacterium Neisseria gonorrhoeae. Uncomplicated gonococcal infection often manifests as urethritis in men and can cause mucopurulent cervicitis in women. Infection with Neisseria gonorrhoeae has a direct effect in facilitating transmission of the human immunodeficiency virus (HIV). Gonorrhea can be cured; however, the pathogen causing the disease produces many mechanisms of resistance to antibiotics, which may be associated with treatment failure. In 2008, the incidence of gonorrhea in Poland was 0.5 per 100,000 population, and this value is over 50 times lower for the same period, compared to the whole of Europe.
Conclusions:
Epidemiological data may indicate an underestimation of the cases of gonorrhea in Poland. The data collected by Polish State institutions indicate that the problem of prevention and diagnosis of diseases transmitted through sexual contact is underfunded.
Sexually transmitted infections are a serious public health problem worldwide, negatively affect the quality of life and cause serious diseases. More than a million sexually transmitted diseases are acquired every day. Despite the high incidence of sexually transmitted diseases, these diseases still remain a neglected area for prevention programmes, diagnostic tests and appropriate treatment. The aim of the study is presentation of the problems associated with Neisseria gonorrhoeae infections
Current state of knowledge:
One of the most common sexually transmitted diseases is gonorrhea, caused by the bacterium Neisseria gonorrhoeae. Uncomplicated gonococcal infection often manifests as urethritis in men and can cause mucopurulent cervicitis in women. Infection with Neisseria gonorrhoeae has a direct effect in facilitating transmission of the human immunodeficiency virus (HIV). Gonorrhea can be cured; however, the pathogen causing the disease produces many mechanisms of resistance to antibiotics, which may be associated with treatment failure. In 2008, the incidence of gonorrhea in Poland was 0.5 per 100,000 population, and this value is over 50 times lower for the same period, compared to the whole of Europe.
Conclusions:
Epidemiological data may indicate an underestimation of the cases of gonorrhea in Poland. The data collected by Polish State institutions indicate that the problem of prevention and diagnosis of diseases transmitted through sexual contact is underfunded.
REFERENCES (55)
1.
Kirkcaldy RD, Weston E, Segurado AC, Hughes G. Epidemiology of gonorrhoea: a global perspective. Sex Health. 2019; 16(5): 401–411. doi: 10.1071/SH19061.
2.
Tacconelli E, Magrini N. Global priority list of antibiotic-resistant bac-teria to guide research, discovery, and development of new antibiotics. Geneva WHO Report; 2017. 8 p.
3.
Freire-Moran L, Aronsson B, Manz C, Gyssens IC, So AD, et al. ECDC--EMA Working Group. Critical shortage of new antibiotics in develo-pment against multidrug-resistant bacteria-Time to react is now. Drug Resist Updat. 2011 Apr; 14(2): 118–24. doi: 10.1016/j.drup.2011.02.00.
4.
Epub 2011 Mar 23.4. Wi T, Lahra MM, Ndowa F, et al. Antimicrobial resistance in Neisseria gonorrhoeae: Global surveillance and a call for international colla-borative action. PLoS Med. 2017, Jul 7; 14(7): e1002344. doi: 10.1371/journal.pmed.1002344.
5.
Brooks GF, Jawetz E, Melnick JL, Adelberg EA. Jawetz, Melnick & Adelberg’s Medical Microbiology. 26th ed. New York, London: McGraw--Hill Medical; 2013.
7.
Tapsall J. Antimicrobial resistance in Neisseria gonorrhoeae, WHO collaborating Centre for STD and HIV. Sydney: World Health; 2001.
8.
Bignell C, Unemo M; European STI Guidelines Editorial Board. 2012 Eu-ropean guideline on the diagnosis and treatment of gonorrhoea in adults. Int J STD AIDS. 2013, Feb; 24(2): 85–92. doi: 10.1177/0956462412472837.
9.
Hill SA, Masters TL, Wachter J. Gonorrhea – an evolving disease of the new millennium. Microb Cell. 2016, Sep 5; 3(9): 371–389. doi: 10.15698/mic2016.09.524.
10.
Mayor MT, Roett MA, Uduhiri KA. Diagnosis and management of gonococcal infections. Am Fam Physician. 2012, Nov 15; 86(10): 931–8. Erratum in: Am Fam Physician. 2013 Feb 1; 87(3): 163.
11.
Unemo M, Shafer WM. Antibiotic resistance in Neisseria gonorrhoeae: origin, evolution, and lessons learned for the future. Ann N Y Acad Sci. 2011, Aug; 1230: E19–28. doi: 10.1111/j.1749- 6632 .2011.06215.x.
12.
Barrow RY, Ahmed F, Bolan GA, Workowski KA. Recommendations for Providing Quality Sexually Transmitted Diseases Clinical Services, 2020. MMWR. Recommendations and Reports: Morbidity and Mor-tality Weekly report. Recommendations and Reports. 2020 Jan; 68(5): 1–20. doi: 10.15585/mmwr.rr6805a1.
13.
Bala M, Sood S. Cephalosporin Resistance in Neisseria gonorrhoeae. J Glob Infect Dis. 2010, Sep; 2(3): 284–90. doi: 10.4103/0974-777X.68537.
14.
Sherrard J, Wilson J, Donders G, Mendling W, Jensen JS. 2018 Euro-pean (IUSTI/WHO) International Union against sexually transmitted infections (IUSTI) World Health Organisation (WHO) guideline on the management of vaginal discharge. Int J STD AIDS. 2018, Nov; 29(13): 1258–1272. doi: 10.1177/0956462418785451. Epub 2018 Jul 27.
15.
European Centre for Disease Prevention and Control. Gonorrhoea. In: ECDC. Annual Epidemiological Report for 2014. Stockholm: ECDC; 2016.
16.
European Centre for Disease Prevention and Control. Gonorrhoea. In: ECDC. Annual epidemiological report for 2015. Stockholm: ECDC; 2 017.
17.
European Centre for Disease Prevention and Control. Gonorrhoea. In: ECDC. Annual Epidemiological Report for 2016. Stockholm: ECDC; 2018.
18.
European Centre for Disease Prevention and Control. Gonorrhoea. In: ECDC. Annual epidemiological report for 2017. Stockholm: ECDC; 2019.
19.
European Centre for Disease Prevention and Control. Gonorrhoea. In: ECDC. Annual epidemiological report for 2018. Stockholm: ECDC; 2020.
20.
European Centre for Disease Prevention and Control. Annual epide-miological report 2014 – food- and waterborne diseases and zoonoses. Stockholm: ECDC; 2014.
21.
68th World Health Assembly. Resolution WHA68.17: contributing to social and economic development: sustainable action across sectors to improve health and health equity (follow-up of the 8th Global Confe-rence on Health Promotion). Progress reports A68/36 Geneva: World Health Organization; 2015.
22.
Zarządzenie Prezesa NFZ z dnia 30 maja 2008 r. w sprawie szcze-gółowych materiałów informacyjnych o przedmiocie postępowania w sprawie zawarcia umów o udzielanie świadczeń opieki zdrowotnej Nr 31/2008/DGL 2008.
23.
Rozporządzenie Ministra Zdrowia z dnia 6 listopada 2013 r. w sprawie świadczeń gwarantowanych z zakresu ambulatoryjnej opieki specjalistycznej (Dz.U. z 2013 r. poz. 1413 z póź. zm.).
24.
Kochanowski J. Pismo Rzecznika Praw Obywatelskich do Ministra Zdrowia z 24 lipca 2008 r.
25.
Kacperczyk-Baran T. Zgłaszalnośc chorów zakaźnych w latach 2000–2004 na terenie działalności PSSEE Zwoleń. Przegl Epidemiol. 2005; 59: 731–737.
26.
Czarkowski MP, Cielebąk E, Kondej B, Sadłocha A. Choroby zakaźne i zatrucia w Polsce w 2010 roku. Biuletyn roczny NIZP-PZH. Warszawa; 2011.
27.
Czarkowski MP, Cielebąk E, Kondej B, Sadłocha A. Choroby zakaźne i zatrucia w Polsce w 2011 roku. Biuletyn roczny NIZP-PZH. Warszawa; 2012.
28.
Czarkowski MP, Cielebąk E, Kondej B, Sadłocha A. Choroby zakaźne i zatrucia w Polsce w 2012 roku. Biuletyn roczny NIZP-PZH. Warszawa; 2013.
29.
Czarkowski MP, Cielebąk E, Kondej B, Sadłocha A. Choroby zakaźne i zatrucia w Polsce w 2013 roku. Biuletyn roczny NIZP-PZH. Warszawa; 2014.
30.
Czarkowski MP, Cielebąk E, Staszewska-Jakubik E, Kondej B. Choroby zakaźne i zatrucia w Polsce w 2014 roku. Biuletyn roczny NIZP-PZH. Warszawa ; 2015.
31.
Czarkowski MP, Cielebąk E, Staszewska-Jakubik E, Kondej B. Choroby zakaźne i zatrucia w Polsce w 2015 roku. Biuletyn roczny NIZP-PZH. Warszawa; 2016.
32.
Czarkowski MP, Cielebąk E, Staszewska-Jakubik E, Kondej B. Choroby zakaźne i zatrucia w Polsce w 2016 roku. Biuletyn roczny NIZP-PZH. Wa r s z aw a ; 2 017.
33.
Czarkowski MP, Cielebąk E, Staszewska-Jakubik E, Kondej B. Choroby zakaźne i zatrucia w Polsce w 2017 roku. Biuletyn roczny NIZP-PZH. Wa rsz awa ; 2018.
34.
Czarkowski MP, Cielebąk E, Staszewska-Jakubik E, Kondej B. Choroby zakaźne i zatrucia w Polsce w 2018 roku. Biuletyn roczny NIZP-PZH. Wa rsz awa ; 2019.
35.
Choroby zakaźne i zatrucia w Polsce w 2019 roku. podstawowe tablice robocze – wstępne dane stan w dniu 15.04.2020 r. Warszawa; 2019.
36.
European Centre for Disease Prevention and Control. Sexually trans-mitted infections in Europe 2013. Stockholm: ECDC; 2015.
37.
Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance 2016. Atlanta: U.S. Department of Health and Human Services; 2017.
38.
World Health Organisation. Global Health Sector Strategy on Sexually Transmitted Infections 2016–2021. Geneva: WHO; 2016.
39.
Centers for Disease Control and Prevention. Carbapenem-Resistant Enterobacteriaceae (CRE) Control and Prevention Toolkit. Rockville: Agency for Healthcare Research and Quality; 2015.
40.
Latini A, Magri F, Donà MG, et al. COVID-19 affecting the epide-miology of STIs? The experience of syphilis in Rome Sexually Trans-mitted Infections. Published Online First: 27 July 2020. doi: 10.1136/sextrans-2020-054543.
41.
Cusini M, Benardon S, Vidoni G, et al. Trend of main STIs during COVID-19 pandemic in Milan, Italy. Sexually Transmitted Infec-tions. Published Online First: 12 August 2020. doi: 10.1136/sex-trans-2020-054608.
42.
Comninos NB, Garton L, Guy R, et al. Increases in pharyngeal Neisseria gonorrhoeae positivity in men who have sex with men, 2011–2015: ob-servational study. Sexually Transmitted Infections. 2020; 96: 432–435.
43.
Żabicka D, Gniadkowski M, Ozorowski T, et al. Raport Krajowego Ośrodka Referencyjnego ds. Lekowrażliwości Drobnoustrojów. Wystę-powanie Enterobacteriaceae (Klebsiella pneumoniae) wytwarzających karbapenemazy typu New Delhi na terenie Polski w I kwartale 2017 roku. Warszawa, 15 czerwca 2017 r.
44.
World Health Organization. (2015). Global action plan on antimicrobial resistance. Geneva: WHO; 2015.
45.
World Health Organization. Draft Global action plan on antimicrobial resistance WHA68.7. Geneva: WHO; 2015.
46.
Bradford PA. Extended-spectrum beta-lactamases in the 21st century: characterization, epidemiology, and detection of this important resi-stance threat. Clin Microbiol Rev. 2001; 14(4): 933–951. doi: 10.1128/CMR.14.4.933-951.2001.
47.
Blomberg B, Jureen R, Manji KP, et al. High rate of fatal cases of pediatric septicemia caused by gram-negative bacteria with extended-spectrum beta-lactamases in Dar es Salaam, Tanzania. J Clin Microbiol. 2005 Feb; 43(2): 745–9. doi: 10.1128/JCM.43.2.745-749.2005.
48.
Paterson DL, Bonomo RA. Extended-spectrum beta-lactamases: a cli-nical update. Clin Microbiol Rev. 2005; 18(4): 657–686. doi: 10.1128/CMR.18.4.657-686.2005.
49.
Sougakoff W, Petit A, Goussard S, et al. Characterization of the plas-mid genes blaT-4 and blaT-5 which encode the broad-spectrum beta--lactamases TEM-4 and TEM-5 in enterobacteriaceae. Gene. 1989, May 30; 78(2): 339–48. doi: 10.1016/0378-1119(89)90236-9.
50.
van Embden JD, van Klingeren B, Dessens-Kroon M, et al. Penicillinase--producing Neisseria gonorrhoeae in the Netherlands: epidemiology and genetic and molecular characterization of their plasmids. Antimicrob Agents Chemother. 1980, Nov; 18(5): 789–97. doi: 10.1128/aac.18.5.789.
51.
Ohnishi M, Ono E, Shimuta K, et al. Identification of TEM-135 beta--lactamase in penicillinase-producing Neisseria gonorrhoeae strains in Japan. Antimicrob Agents Chemother. 2010 Jul; 54(7): 3021–3. doi: 10.1128/AAC.00245-10. Epub 2010 Apr 26.
52.
Gianecini R, Oviedo C, Guantay C, et al. Prevalence of bla TEM-220 gene in Penicillinase-producing Neisseria gonorrhoeae strains carrying Toronto/Rio plasmid in Argentina, 2002–2011. BMC Infect Dis. 2015, Dec 16; 15: 571. doi: 10.1186/s12879-015-1294-0.
53.
Unemo M, Shafer WM. Antimicrobial resistance in Neisseria go-norrhoeae in the 21st century: past, evolution, and future. Clin Microbiol Rev. 2014 Jul; 27(3): 587–613. doi: 10.1128/CMR.00010-14.
54.
Muhammad I, Golparian D, Dillon JA, et al. Characterisation of blaTEM genes and types of β-lactamase plasmids in Neisseria gonorrhoeae – the prevalent and conserved blaTEM-135 has not recently evolved and existed in the Toronto plasmid from the origin. BMC Infect Dis. 2014, Aug 22; 14: 454. doi: 10.1186/1471-2334-14-454.
55.
Arlet G, Goussard S, Courvalin P, et al. Sequences of the genes for the TEM-20, TEM-21, TEM-22, and TEM-29 extended-spectrum beta--lactamases. Antimicrob Agents Chemother. 1999, Apr; 43(4): 969–71.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.