RESEARCH PAPER
Prevalence of modifiable cardiovascular risk factors in patients hospitalized due to symptomatic coronary artery disease in the Lublin Province
1
Wojewódzki Szpital Specjalistyczny im. Stefana Kardynała Wyszyńskiego w Lublinie, Polska
2
Instytut Medycyny Wsi, Lublin, Polska
Corresponding author
Anna Ilona Gózd-Barszczewska
Wojewódzki Szpital Specjalistyczny im. Stefana Kardynała Wyszyńskiego w Lublinie, Al. Kraśnicka 100, 20-718, Lublin, Polska
Wojewódzki Szpital Specjalistyczny im. Stefana Kardynała Wyszyńskiego w Lublinie, Al. Kraśnicka 100, 20-718, Lublin, Polska
Med Og Nauk Zdr. 2021;27(4):453-560
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Despite the enormous advances in cardiology made in recent decades, ischaemic heart disease (IHD) remains one of the most important health problems in highly developed countries, including Poland. An attempt was made to identify the most common risk factors for IHD based on the analysis of medical records of patients hospitalized due to the symptomatic coronary artery disease to intensify the preventive measures in the Lublin Province.
Material and methods:
All males aged 45–65 hospitalized in the Cardiology Ward with the Cardiac Intensive Care Unit at the Cardinal Stefan Wyszyński Hospital in Lublin in the period from 1 January 2016 – 10 March 2017 due to symptomatic stable angina or acute coronary syndrome were qualified for the study. The studygroup included 142 patients. Based on medical records, the prevalence of modifiable risk factors for IHD was determined. The obtained data were statistically analysed.
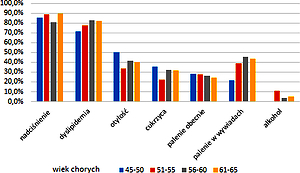
Results:
The presence of modifiable cardiovascular risk factors was common, and the most frequently diagnosed were: dyslipidemia and arterial hypertension. A positive correlation was found between an increase in body mass index, and the diagnosis of diabetes (p<0.001) and arterial hypertension (p=0.003). In patients without history of IHD, acute coronary syndromes were diagnosed significantly more often than stable angina (p <0.001).
Conclusions:
The obtained results indicate that due to the prevalence of modifiable cardiovascular risk factors, efforts should be made to intensify primary and secondary prevention programmes. Special measures should be aimed at the proper treatment of hypertension and dyslipidemia, and the struggle against obesity should also be a priority. One of the key aspects of preventive actions should be intensive education on the methods of prevention and early elimination of the existing threats.
Despite the enormous advances in cardiology made in recent decades, ischaemic heart disease (IHD) remains one of the most important health problems in highly developed countries, including Poland. An attempt was made to identify the most common risk factors for IHD based on the analysis of medical records of patients hospitalized due to the symptomatic coronary artery disease to intensify the preventive measures in the Lublin Province.
Material and methods:
All males aged 45–65 hospitalized in the Cardiology Ward with the Cardiac Intensive Care Unit at the Cardinal Stefan Wyszyński Hospital in Lublin in the period from 1 January 2016 – 10 March 2017 due to symptomatic stable angina or acute coronary syndrome were qualified for the study. The studygroup included 142 patients. Based on medical records, the prevalence of modifiable risk factors for IHD was determined. The obtained data were statistically analysed.
Results:
The presence of modifiable cardiovascular risk factors was common, and the most frequently diagnosed were: dyslipidemia and arterial hypertension. A positive correlation was found between an increase in body mass index, and the diagnosis of diabetes (p<0.001) and arterial hypertension (p=0.003). In patients without history of IHD, acute coronary syndromes were diagnosed significantly more often than stable angina (p <0.001).
Conclusions:
The obtained results indicate that due to the prevalence of modifiable cardiovascular risk factors, efforts should be made to intensify primary and secondary prevention programmes. Special measures should be aimed at the proper treatment of hypertension and dyslipidemia, and the struggle against obesity should also be a priority. One of the key aspects of preventive actions should be intensive education on the methods of prevention and early elimination of the existing threats.
REFERENCES (43)
1.
Cierniak-Piotrowska M, Marciniak G, Stańczak J. Zachorowalność i umieralność na choroby układu krążenia a sytuacja demograficzna Polski. https://stat.gov.pl/obszary-te... (access: 2020.10.02).
2.
Podolec P, Kopeć G, Pająk A. Czynniki ryzyka chorób sercowo-naczyniowych. In: Podręcznik Polskiego Forum Profilaktyki Tom I. Medycyna Praktyczna 2007. p. 83–87.
3.
Williams B, Mancia G, Spiering W, et al. 20018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018; 39(33): 3012–3104. https://doi.org/10.1093/eurhea....
4.
Narodowy Program Profilaktyki i Rozwiązywania Problemów Alkoholowych na lata 2011–2015. https://www.parpa.pl/images/im... (access: 2019.01.21).
5.
Szymański FM, Barylski M, Cybulska B, et al. Recommendation for the management of dyslipidemia in Poland – Third Declaration of Sopot. Interdisciplinary Expert Position Statement endorsed by the Polish Cardiac Society Working Group on Cardiovascular Pharmacotherapy. Cardiol J. 2018; 25(6): 655–665. https://doi.org/10.5603/CJ.201....
6.
Czupryniak L. Zalecenia kliniczne Polskiego Towarzystwa Diabetologicznego dotyczące postępowania u chorych na cukrzycę – najważniejsze zmiany na rok 2018. Med Prakt. 2018; 4: 43–48.
7.
Radovanovic CAT, dos Santos LA, Carvalho MDB, et al. Arterial Hypertension and other risk factors associated with cardiovascular diseases among adults. Rev Lat Am Enfermagem. 2014; 22(4): 547–553. https://doi.org/10.1590/0104-1....
8.
Dua S, Bhuker M, Sharma P, et al. Body Mass Index Relates to Blood Pressure Among Adults. N Am J Med Sci. 2014; 6(2): 89–95. https://doi.org/10.4103/1947-2....
9.
Kotsis V, Stabouli S, Papakatsika S, et al. Mechanisms of obesity-induced hypertension. Hypertens Res. 2010; 33(5): 386–393. https://doi.org/10.1038/hr.201....
10.
Zdrojewski T, Drygas W, Naruszewicz M, et al. Nadciśnienie tętnicze w populacji ogólnej. In: Więcek A, Januszewicz A, Szczepańska-Sadowska E, Narkiewicz K, Prejbisz A, Cudnoch-Jędrzejewska A. Hiperten sjologia. Patogeneza, diagnostyka i leczenie nadciśnienia tętniczego. Medycyna Praktyczna. Wyd. 2. Kraków; 2015. p. 1–17.
11.
Niklas A, Flotyńska A, Puch-Walczak A, et al. Prevalence, awareness, treatment and control of hypertension in the adult Polish population Multi-center National Population Health Examination Surveys – WOBASZ studies. Arch Med Sci. 2018; 14(5): 951–961. https://doi.org/10.5114/aoms.2....
12.
Pająk A, Szafraniec K, Polak M, et al. Changes in the prevalence, treatment, and control of hypercholesterolemia and other dyslipidemias over 10 years in Poland: the WOBASZ study. Pol Arch Med Wewn. 2016; 126(9): 642–652. https://doi.org/10.20452/pamw.....
13.
Zdrojewski T, Solnica B, Cybulska B, et al. Prevalence of lipid abnormalities in Poland. The NATPOL 2011 survey. Kardiol Pol. 2016; 74(3): 213–223. https://doi.org/10.5603/KP.201....
14.
Abd alamir M, Goyfman M, Chaus A, et al. The Correlation of Dyslipidemia with the Extent of Coronary Artery Disease in the Multiethnic Study of Atherosclerosis. J Lipids. 2018; 2018: 5607349. https://doi.org/10.1155/2018/5....
15.
Chou R, Dana T, Blazina I, et al. Statins for Prevention of Cardiovascu-lar Disease in Adults: Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA. 2016; 316(19): 2008–2024. https://doi.org/10.1001/jama.2....
16.
Ference BA, Ginsberg HN, Graham I, et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European Atherosclerosis Society Consensus Panel. Eur Heart J. 2017; 38(32): 2459–2472. https://doi.org/10.1093/eurhea....
17.
Unamuno X, Gómez-Ambrosi J, Rodríguez A, et al. Adipokine dysregulation and adipose tissue inflammation in human obesity. Eur J Clin Invest. 2018; 48(9): e12997. https://doi.org/10.1111/eci.12....
18.
Emerging Risk Factors Collaboration, Wormser D, Kaptoge S, Di Angelantonio E, et al. Separate and combined associations of body-mass index and abdominal adiposity with cardiovascular disease: collaborative analysis of 58 prospective studies. Lancet. 2011; 377(9771): 1085–1095. https://doi.org/10.1016/S0140-....
19.
Piepoli MF, Hoes AW, Agewall S, et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts) Developed with the special contribution of the European Association for Cardiovas cular Prevention & Rehabilitation (EACPR). Eur Heart J. 2016; 37(29): 2315–2381. https://doi.org/10.1093/eurhea....
20.
Hippisley-Cox J, Coupland C, Vinogradova Z, et al. Predicting car-diovascular risk in England and Wales: prospective derivation and validation of QRISK2. BMJ. 2008; 336 (7659): 1475–1482. https://doi.org/10.1136/bmj.39....
21.
Stan zdrowia ludności Polski w 2014 r. www.stat.gov.pl/obszary-tema-tyczne/zdrowie/zdrowie/stan-zdrowia-ludnosci-polski-w-2014-r-,6,6.html (access: 2018.10.07).
22.
Stepaniak U, Micek A, Waśkiewicz A, et al. Prevalence of general and abdominal obesity and overweight among adults in Poland. Results of the WOBASZ II study (2013–2014) and comparison with the WOBASZ study (2003–2005). Pol Arch Med Wewn. 2016; 126(9): 662–671. https://doi.org/10.20452/pamw.....
23.
Surma S, Szyndler A, Narkiewicz K. Świadomość nadciśnienia tętnicze-go i innych czynników ryzyka chorób układu sercowo-naczyniowego w populacji osób dorosłych. Choroby Serca i Naczyń 2018; 15(1): 14–22.
24.
Muszyński J, Żółtańska J, Michalczak W, et al. Analiza stylu życia doro-słych mieszkańców Dolnego Śląska w aspekcie zapobiegania chorobom sercowo-naczyniowym. Fam Med Prim Care Rev. 2016; 18(1): 33–38. https://doi.org/10.5114/fmpcr/....
25.
Zdrojewski T, Rutkowski M, Bandosz P, et al. Ocena rozpowszechnienia i kontroli czynników ryzyka chorób serca i naczyń w Polsce – badania NATPOL 1997, 2002, 2011. In: Kopeć G, Jankowski P, Pająk A, Drygas W. Epidemiologia i prewencja chorób układu krążenia. Kraków: Medycyna Praktyczna; 2015. p. 57–64.
26.
Rutkowski M, Bandosz P, Czupryniak L, et al. Prevalence of diabetes and impaired fasting glucose in Poland — the NATPOL 2011 Study. Diabet Med. 2014; 31(12): 1568–1571. https://doi.org/10.1111/dme.12....
27.
Drygas W, Bielecki W, Kozakiewicz K, et al. Wieloośrodkowe Ogólnopolskie Badanie Stanu Zdrowia Ludności – WOBASZ. In: Kopeć G, Jankowski P, Pająk A, Drygas W. Epidemiologia i prewencja chorób układu krążenia. Kraków: Medycyna Praktyczna; 2015. p. 41–56.
28.
Klimek M, Knap J, Tulwin T, et al. Evaluation of the relationship be-tween the prevalence of diabetes and selected demographic factors. Clin Diabetol. 2018; 7(3): 145–150. https://doi.org/10.5603/DK.201....
29.
Bays HE, Chapman RH, Grandy S, the SHIELD Investigators’ Group. The relationship of body mass index to diabetes mellitus, hypertension and dyslipidaemia: comparison of data from two national surveys. Int J Clin Pract. 2007; 61(5): 737–747. https://doi.org/10.1111/j.1742....
30.
Einarson TR, Acs A, Ludwig C, et al. Prevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence from across the world in 2007–2017. Cardiovasc Diabetol. 2018; 17: 83. https://doi.org/10.1186/s12933....
31.
Swift DL, Houmard JA, Slentz CA, et al. Effects of aerobic training with and without weight loss on insulin sensitivity and lipids. PLoS One. 2018; 13(5): e0196637. https://doi.org/10.1371/journa....
32.
Zdrojewski T, Rutkowski M, Bandosz P. Epidemiologia palenia papierosów oraz innych czynników ryzyka chorób układu krążenia w Polsce – badanie NATPOL 2011. IV konferencja „Tytoń albo Zdrowie” im. prof. F. Venuleta; 2011 Gru 09; Warszawa, Polska.
33.
Vartiainen E. The North Karelia Project: Cardiovascular disease prevention in Finland. Glob Cardiol Sci Pract. 2018 Jun; 2018(2): 13. https://doi.org/10.21542/gcsp.....
34.
Knuuti J, Wijns W, Saraste A, et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes: The Task Force for the diagnosis and management of chronic coronary syndromes of the European Society of Cardiology (ESC). Eur Heart J. 2020; 41(3): 407–477. https://doi.org/10.1093/eurhea....
35.
Haro C, Rangel-Zúñiga OA, Alcalá-Díaz JF, et al. Intestinal Microbiota Is Influenced by Gender and Body Mass Index. PLoS One. 2016; 11(5): e0154090. https://doi.org/10.1371/journa....
36.
Turnbaugh PJ, Hamady M, Yatsunenko T, et al. A core gut microbiome in obese and lean twins. Nature. 2009; 457(7228): 480–484. https://doi.org/10.1038/nature....
37.
Allayee H, Hazen SL. Contribution of Gut Bacteria to Lipid Levels: Another Metabolic Role for Microbes?. Circ Res. 2015; 117(9): 750–754. https://doi.org/10.1161/CIRCRE....
38.
Fu J, Bonder MJ, Cenit MC, et al. The Gut Microbiome Contributes to a Substantial Proportion of the Variation in Blood Lipids. Circ Res. 2015; 117(9): 817–824. https://doi.org/10.1161/CIRCRE....
39.
Gózd-Barszczewska A, Kozioł-Montewka M, Barszczewski P, et al. Gut microbiome as a biomarker of cardiometabolic disorders. Ann Agric Environ Med. 2017; 24(3): 416–422. https://doi.org/10.26444/aaem/....
40.
Jie Z, Xia H, Zhong SL, et al. The gut microbiome in atherosclerotic cardiovascular disease. Nat Commun. 2017; 8(1): 845. https://doi.org/10.1038/s41467....
41.
Pluznick JL, Protzko RJ, Gevorgyan H, et al. Olfactory receptor respon-ding to gut microbiota-derived signals plays a role in renin secretion and blood pressure regulation. Proc Natl Acad Sci U S A. 2013; 110(11): 4410–4415. https://doi.org/10.1073/pnas.1....
42.
Yang T, Santisteban MM, Rodriguez V, et al. Gut microbiota dysbiosis is linked to hypertension. Hypertension. 2015; 65(6): 1331–1340. https://doi.org/10.1161/HYPERT....
43.
Larsen N, Vogensen FK, van den Berg FW, et al. Gut Microbiota in Human Adults with Type 2 Diabetes Differs from Non-Diabetic Adults. PLoS One. 2010; 5(2): e9085. https://doi.org/10.1371/journa....
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.